Donated tumor tissue from a 5-year-old brain cancer patient uncovers the key and early role of a less-understood genetic mutation in the cancer’s fatal course.
11:00 AM
Author |

A year and a half after losing his battle against brain cancer, Chad Carr's legacy lives through research that will help other children facing the same cruel disease.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Chad, the grandson of former University of Michigan football coach Lloyd Carr, died at age 5 in 2015, 14 months after being diagnosed with the most aggressive and lethal type of brain tumor, diffuse intrinsic pontine glioma (DIPG).
Now, Chad's donated tumor tissue is offering researchers new insight into the genetic mutations that drive DIPG to grow and progress. The first study based on his tumor appears in Nature's npj Precision Oncology.
"Typically with a biopsy, we get a single snapshot of the genetic characteristics of the tumor. That doesn't always give you an accurate picture because each region of the tumor may be driven by different genetic changes," says lead author Carl Koschmann, M.D., a pediatric oncologist at U-M's C.S. Mott Children's Hospital.
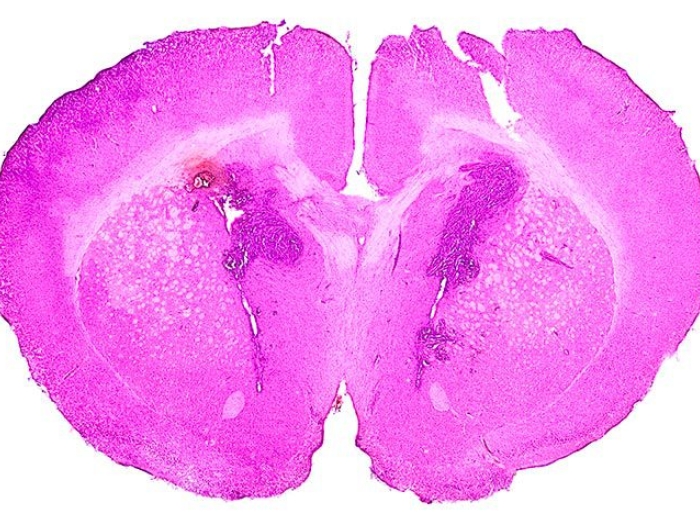
"In this case, we were able to sequence and analyze samples from one time point from six different regions of the tumor — which gives us an incredibly rich resource of what we can learn from one DIPG. This goes much further in telling the genetic life story of the tumor."
The research, supported by Michigan Medicine's Pediatric Brain Tumor Research Initiative, establishes that a mutation in a gene known as PTEN — not previously seen as a major DIPG driver — plays an early and important role in DIPG's fatal course. The project was a result of the collaboration of DIPG research among pediatrics, neurosurgery and pathology at Michigan Medicine.
"This was Chad's final physical gift, and to see that gift making a difference to DIPG research that will someday change the future for other children means so much to us," says Chad's mom, Tammi Carr.

PTEN's influence
In a normal cell, the PTEN gene plays an integral role in suppressing cancer, killing cells that aren't behaving the way they're supposed to. Any loss or mutation of the gene makes the tumor more effective.
SEE ALSO: DIPG Disruptors: 6 New Brain Tumor Research Efforts Underway
But PTEN has not historically been considered a key driver of DIPG in children, and it remains unclear how early or "clonal" it is in the development of these tumors. Mutations that are seen throughout multiple regions in a tumor are considered crucial events in the earliest clusters, or clones, of cancer cells. These clonal events lead to widespread changes in the tumor that may provide ideal targets for precision medicine therapies.
Koschmann says the new data add to compelling evidence suggesting that PTEN should be considered in treatment decisions. Researchers also analyzed data from the PedcBioPortal, a national set of pediatric cancer genomics data, and found alterations in PTEN in up to 5 percent of DIPG cases.
This is frequent enough to show it's a recurring mutation, Koschmann says.
"PTEN has not historically been considered one of the major four mutations of DIPG. However, we found a mutation in both copies of PTEN in every single region of Chad's tumor, which was unexpected. These findings have unearthed the gene mutation's key and early role in DIPG development," says Koschmann.
"This study strengthens the case that alterations of the PTEN gene play a more influential role than was previously understood and should be included in future sequencing panels for pediatric DIPG," he adds. "If we find it, it's something we can hopefully target with precision therapy."
While some gene mutations don't yet have a drug that targets them, PTEN has been targeted in breast and prostate cancer, Koschmann says, which is why it may benefit future DIPG patients.
Sequencing Chad's 4.6-centimeter tumor in multiple regions allowed researchers to clarify how the DIPG behaved in each location of the brain and brain stem. It's an example of how this type of data can help create an "evolutionary map" of the tumor, Koschmann says.
"We are able to look at what DIPG looks like after it's been through traditional therapy and learning how the tumor grew and evaded those treatments," Koschmann says. "Studying tumor tissue in this way is like reading a textbook on how the tumor evolved after treatments and how we may potentially cut that off in the future."
The new genetic information we gain from studies like this will help us get closer to developing a new approach to treating children with what is now an incurable disease.Carl Koschmann, M.D.
Building momentum
Tumor tissue donations in pediatric cancer cases have historically been rare because they need to happen just hours after death. Doctors are not likely to even broach the topic with families. Michigan researchers say that since the Carr story gained national attention, more families have asked for biopsies or autopsies of tumors.
Chad's story galvanized the community, inspiring the #ChadTough movement and U-M Chad Tough Fund. This study is the first of several expected to be published as the momentum for DIPG research builds.
It's all part of Chad's legacy, Tammi Carr says.
"We knew from early on in Chad's journey that we would do whatever we could to create change, and we knew Chad would be a part of that change," she says.
"To now see all of the work that has been done in DIPG research and the discoveries that have been made, we are seeing Chad's gift having an incredible impact."
Brain tumors are the leading cause of death from childhood cancer. The most devastating type is DIPG, which stems from the region of the brain that controls breathing and heart rate. More than 90 percent of children diagnosed with DIPG die within 18 months.
"The current prognosis for DIPG remains bleak despite hundreds of previous clinical trials," Koschmann says. "A deeper molecular understanding of each individual tumor is needed to guide therapeutic decisions.
"As we see more funding and more interest in DIPG research, we are learning more each day. The new genetic information we gain from studies like this will help us get closer to developing a new approach to treating children with what is now an incurable disease."
Learn more about the Michigan Medicine Pediatric Brain Tumor Research Initiative.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!