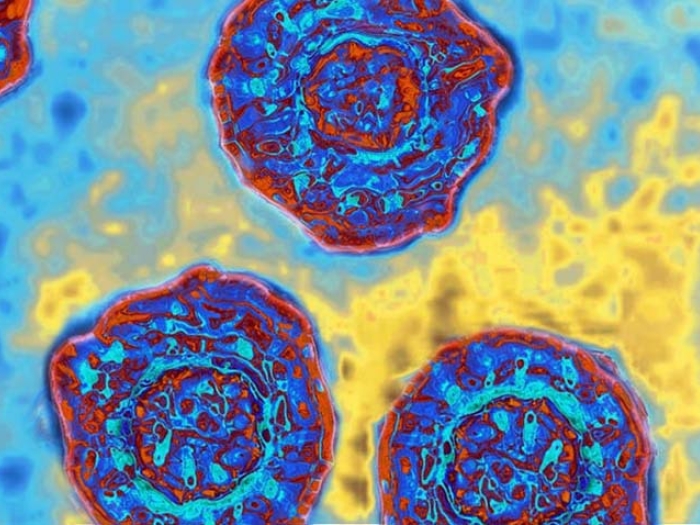
When it comes to the hepatitis C virus (HCV) infection, the treatment landscape has shifted in the past few years. But patients need new models of detection to benefit from better treatments.
3:00 PM
Author |

When it comes to the hepatitis C virus (HCV) infection, the treatment landscape has shifted in the past few years.
All-oral combinations of direct-acting antiviral agents (DAAs) have replaced the traditional combination of interferon and ribavirin, which was associated with many side effects. That's good news for the 2 percent to 3 percent of individuals in the United States affected by the disease, per the Centers for Disease Control and Prevention.
"Our group published the first paper in 2012 showing that it is possible to cure HCV infection without the use of interferon," says Anna Suk-Fong Lok, M.D., a hepatologist at the University of Michigan Health System.
Now, Dr. Lok's group is evaluating different combinations of DAAs to identify a regimen that could potentially shorten the duration of treatment, improve cure rates in patients with advanced disease, and be effective for all patient populations and all genotypes of HCV.
But even the best treatments for HCV can reach their full potential only when initiated early in the course of the disease.
"We now have highly effective treatments that can cure hepatitis C in approximately 95 percent of patients who are diagnosed early," says Lok. "But the success rate is lower —less than 90 percent — when diagnosis occurs in the late stages of cirrhosis. Moreover, cure during the early stages of infection eliminates the risk for liver cancer, whereas cure after a patient has already progressed to cirrhosis decreases, but does not eliminate, that risk."
Early diagnosis of HCV infection, therefore, is paramount to avoiding the serious complications of liver disease.
The challenges of early diagnosis
HCV infection can be difficult to detect, for several reasons.
"Many early symptoms of HCV infection, such as fatigue and joint pain, are non specific and may not catch the attention of patients or their doctors." Furthermore, Lok adds, "most patients with hepatitis C do not have any symptoms until they have cirrhosis — and even when they have early cirrhosis, they may not have symptoms."
As a result, many individuals with HCV infection don't even know they are infected. Dr. Lok adds that screening for high-risk groups in particular needs to be improved, so they can benefit from new treatments.
One of Dr. Lok's current research projects addresses this very issue. Working with MiChart,the University of Michigan's electronic health record system, Dr. Lok's team placed electronic alerts indicating the need for HCV testing in all patients born between 1945 and 1965 — a group that is five times more likely to be infected — who have never been tested. The alert links to an order set and provides educational information on HCV infection for primary care physicians, medical staff and patients.
"We just completed the pilot phase of this study, and we observed a marked increase in screening rates," Dr. Lok says.
Her team had feared the addition of yet another alert would cause annoyance on the part of physicians and anxiety on the part of their patients. Instead, "primary care physicians felt that this was one of the best alerts rolled out," she says. As the alert is rolled out more widely, her team will continue to track progress and results.
Our models use novel statistical methods, including machine learning, which allow us to incorporate many more pieces of data compared with traditional models.Anna Suk-Fong Lok, M.D.
A model for disease progression
During the course of HCV infection, some patients progress to liver fibrosis and liver cancer, while others do not. Dr. Lok's team is also analyzing factors associated with this progression.
They are developing "dynamic" models to predict the risk for liver fibrosis progression. Traditional models use data collected from patients at the time of disease presentation, Dr. Lok explains. Dynamic models account for changes over time by using not only baseline data but also longitudinal data. The use of dynamic models allows researchers to adjust risk calculations depending on an individual's course of disease.
"Our models use novel statistical methods, including machine learning, which allow us to incorporate many more pieces of data compared with traditional models. We have found that these dynamic models are more accurate than baseline models in predicting the risk for liver failure and death."
Dr. Lok hopes these models can be refined to be able to predict even earlier stages of liver disease, such as progression from mild to moderate fibrosis.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!