Clues suggest anti-inflammatory macrophages are different in people with diabetes.
9:20 AM
Author |

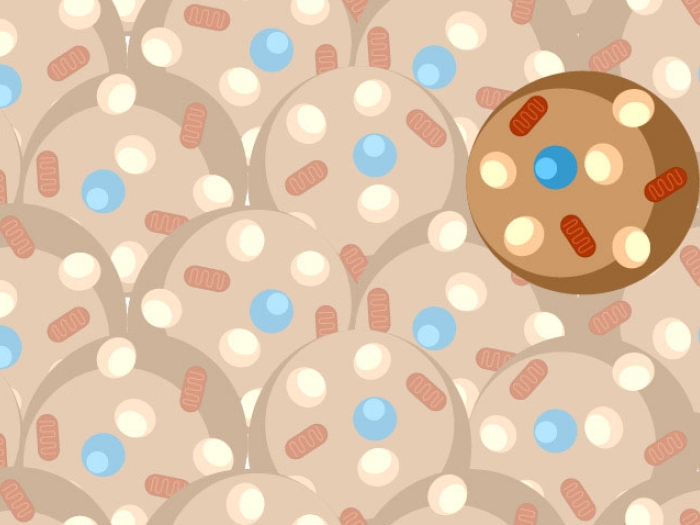
The link between obesity and illness, particularly type 2 diabetes, is well known. Yet researchers are actively working to understand what it is about fat tissue that leads to metabolic disease. Studies in mice have shown that an increase in immune cells called macrophages in fat tissue causes insulin resistance, a precursor to diabetes. Macrophages gobble up foreign material, break it down and help other immune cells determine whether that material is a threat.
Lindsey Muir, Ph.D., research assistant professor with the Department of Computational Medicine and Bioinformatics, and teams in the laboratories of Robert O'Rourke, M.D, and Carey Lumeng, M.D., Ph.D., at the University of Michigan Medical School examined whether fat from humans followed the same pattern.
"Our overarching question is how immune cell types in fat are changing," said Muir. One observation made via mouse studies of obesity is that macrophages change a lot within fat tissue, increasing in number and skewing away from a normal proportion of different types. Furthermore, diabetes combined with obesity also is reflected in changes in macrophages.
Like Podcasts? Add the Michigan Medicine News Break on iTunes, Google Podcasts or anywhere you listen to podcasts.
To study this, the team took fat tissue from patients undergoing bariatric surgery and analyzed the immune cells, specifically macrophages. They divided the cells into three subpopulations, using flow sorting to isolate them—CD206+, which are usually anti-inflammatory; CD11c+, which are usually proinflammatory; and a mix of the two. They wanted to see if there was a correlation between the type of macrophage present in fat tissue and diabetes.
They found that fat from people with diabetes contained more macrophages overall. Interestingly, there appeared to be a strong correlation with CD206+, which Muir explained "is a little counter to what was found in mice."
In mice, CD11c+ appeared to cause diabetes, while in people that subtype was not correlated with the condition. "There could be other subtypes or factors we don't understand about the division of macrophage subtypes," said Muir. Yet, she explained, there is a hint that there is something different within the population of macrophages in people who had diabetes.
To get at this in finer detail they isolated each type and ran population RNA sequencing on three samples of each to look at similarities and differences. They found that CD206+ was not only correlated with diabetes but also highly unique in terms of gene expression when compared to the other two types of macrophages.
"This could indicate a unique function in those cells, which could be contributing to the development of diabetes or at least responding differently in diabetes compared to non-diabetes."
One possible difference, explains Muir, was in the way in which the macrophages engulf particles.
Muir and team then looked at other data available in the field to see if there was overlap among cell types and found significant overlap with anti-inflammatory immune cells found by other researchers. The role of anti-inflammatory cells in disease has been controversial, said Muir, however "if these cells can't monitor and clean up tissue well, it contributes to tissue dysfunction, perhaps as much as if there was too much inflammation."
The differently expressed genes in CD206+ macrophages corresponded with different immune functions including antigen presentation (the way innate immune cells present threats to the adaptive immune cells, known to be important to the development of diabetes in mice), and with the metabolism of lipids.
"Using these bioinformatics methods to categorize sets of genes allows us to check to see if a type or set of genes might be making a functional difference."
Ideally, says Muir, these findings will be backed up with single cell RNA sequencing to take an unbiased look at each cell individually to understand whether there are more immune cell subtypes, how to classify them and then see whether they respond differently in cell culture in the presence of obesity.
Additional authors on the paper include Kae Won Cho, Lynn M. Geletka, Nicki A. Baker, Carmen G. Flesher, Anne P. Ehlers, Niko Kaciroti, Stephen Lindsly, Scott Ronquist, Indika Rajapakse, O'Rourke and Lumeng.
Paper cited: "Human CD206+ macrophages associate with diabetes and adipose tissue lymphoid clusters," JCI Insight. DOI: 10.1172/jci. insight.146563

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!