A Study On Gender Disparities
Fourth-year radiation oncology resident Dr. Jamie Takayesu, discusses her research on whether health care providers talk to women receiving radiation for genitourinary cancer about sexual health and function as much as they do men. Listen to her break down the multifaceted disparity and suggests some potential solutions to bridge the gap.
Transcript
Speaker 1:
Welcome to the Cancer Wise Podcast, where we'll discuss cancer prevention, treatments, the latest in research, and important news around cancer. Brought to you by the University of Michigan Health, Rogel Cancer Center.
Mary Clare Fischer:
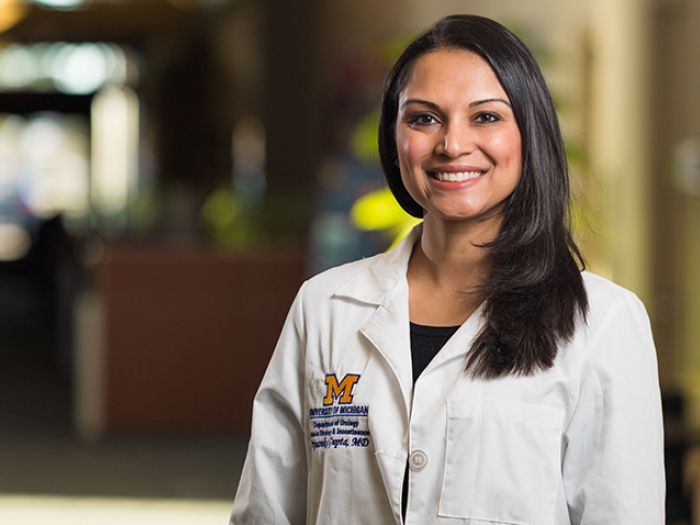
Hello all, and welcome to this episode of Cancer Wise. My name is Mary Clare Fischer, and I'm a public relations representative for the Rogel Cancer Center. One of the most important cancer conferences of the year, The American Society for Radiation Oncology's Annual meeting kicked off this week. And many of our faculty and trainees are giving presentations at this year's event. That includes Dr. Jamie Takayesu, a fourth year radiation oncology resident at University of Michigan Health, who led research examining whether there were disparities in physicians' assessment of sexual dysfunction for women versus men who are receiving brachytherapy for genitourinary cancers. We're lucky enough to have Dr. Takayesu on the show today to talk about her work. So welcome, Dr. Takayesu.
Dr. Jamie Takayesu:
Thank you. Glad to be here.
Mary Clare Fischer:
I wondered if you could start by explaining what brachytherapy is and which patients it's appropriate for.
Dr. Jamie Takayesu:
So brachytherapy is one of the tools that we use as radiation oncologists. And while most of the radiation that we deliver is all external beam radiation coming from the outside, brachytherapy is a much more focused kind of radiation that we deliver internally. And the benefit being that we are giving really [00:01:30] high doses of radiation to the tumor while giving very low doses of radiation to the surrounding normal structures. So, it's quite commonly used in the prostate space. It's pretty much standard of care for most of the gynecologic malignancies with women with more advanced disease.
Mary Clare Fischer:
And what prompted you to dig into these potential disparities around sexual dysfunction assessment for patients receiving brachytherapy?
Dr. Jamie Takayesu:
Honestly, most of this came from my clinical experience. I think prostate cancer is one of the most common cancers, and so we see a lot of it during training. And we get very used to talking to men about their sexual health before radiation and afterwards. And honestly, that's kind of multifaceted because radiation can impact sexual health in men, but a lot of men are also on hormone therapies, which can also impact their sexual health.
But when I went to my gynecologic service, I noticed that I was really not having that same conversation with women. Whereas with men, I would have a very standardized script and I would ask them very standardized questions and give them standardized counseling for every single consult. I didn't have that quite as readily in my mind. And I think I had one patient in particular who was very concerned about her sexual wellbeing after radiation. And I just felt so unequipped to counsel her or to help her.
One of my mentors, Dr. Shruti Jolly, she's fantastic. She's one of the main gynecologic attendings in the radiation oncology department. And she had done a study with Dr. Christina Chapman, also who did residency in our department. And they had actually showed that two thirds of women want to be regularly asked about their sexual function. And that just didn't seem to mesh well with what I had been experiencing in clinic. And I know that over 90% of women will have some kind of sexual dysfunction after surgery and radiation. And it's kind of a lot of damage on the sexual organs. And so, it's really that experience that kind of pushed me to look at the disparities between men and women. And I was pretty surprised to find exactly how big that disparity was with this study.
Mary Clare Fischer:
Yeah. What were some of the most significant takeaways from this research?
Dr. Jamie Takayesu:
So, what we did for this study is, look at all of the consults that came in through our radiation oncology department, both within the prostate brachytherapy realm as well as the gynecologic brachytherapy realm. And I specifically was focusing on the younger female population. Cervical cancer specifically, affects slightly younger demographic compared to uterine cancers, and that was quite intentional. Whereas, prostate cancer can affect a wider age of men, but typically, affects men of an older age.
And 13% of women were asked about their sexual function at the time of consult, versus 90% of men who were undergoing or were being consulted on brachytherapy. I mean, that is a huge difference. I think we do a little bit better in the return visit setting. We do ask about women's sexual function more regularly. But I think that consult time is such an important time to kind of set the tone for how the rest of your follow up is going to go. It's an important time to discuss what the patients are most concerned about, and clearly we're not doing a really good job for women, frankly.
I think this is multifaceted again, and might have to do with the fact that men with prostate cancer in general have a better prognosis than women with cervical cancer. But again, I think it's still a big disparity that kind of raised a lot of questions in my mind. And so I think my first question was, is this just a phenomenon at our institution or is this a national issue? And I don't really have access to every hospital's database, but I did have access to the clinical trials that are run across the country.
And so, we looked at all the NIH funded studies, clinical trials that had happened and are ongoing currently. And we still see that same disparity, whereas 17% of clinical trials run for men with prostate cancer who were going to be treated with brachytherapy. So, 17% of those trials look at sexual function and kind of formally assess the question about sexual function. Only 6% of trials in the cervical cancer [00:06:30] space asks those same questions about sexual function. So it does seem like a national problem, not just an institutional problem.
Mary Clare Fischer:
I love the fact that you looked at one center, but then also kind of broadened this to more clinical trials to make sure that this wasn't an isolated problem. And I wonder if you could speak to, what do you think this says about how women and particularly women's sexual lives and function are prioritized, or maybe clearly not?
Dr. Jamie Takayesu:
Yeah. So to be very fair, again, I do think this is multifaceted. It's not just physician bias, it's not just bias of clinical investigators. For men with prostate cancer, they do have a choice of therapy, a lot of times. They can choose between brachytherapy, external beam radiation, surgery. They have a lot of choices, and all [00:07:30] of those impact their sexual function differently. And so certainly, I see the impetus for sexual function research in particularly. Whereas for women with cervical cancer, the treatment paradigm is a little bit more fixed, and they don't quite have those options in their treatment.
However, I do think that there is still a component of societal bias and physician bias, and people just [00:08:00] being uncomfortable with talking about female sexuality. I think another big problem is that for men, we have multiple medications to help with erectile dysfunction. And for women, there's no real silver bullet like there is for men. And so it's a really arduous task actually, to help rehabilitate women to regain their sexual function. It has a lot to do with cognitive [00:08:30] behavioral therapy and physical therapy, pelvic floor therapy. It's a much more complex treatment.
And so, I think there are quite a few barriers for the physician who's not an expert in that. And you're not going to be able to counsel your patients as well. It's not as easy as prescribing a pill. So, I think it's a lot of different factors that are just playing off each other and making it harder for women to get the care that they need.
Mary Clare Fischer:
Was there anything in these results that surprised you?
Dr. Jamie Takayesu:
I think unfortunately, these results didn't surprise me all that much. It really just reinforced all of the clinical scenarios and assumptions that I had, that women were not being asked about their sexual function at the same rate as men. But I think just seeing the numbers and having some kind of quantity to compare, really, that was striking for our gynecologic team to just see those numbers.
Since this abstract has gotten kind of passed around our department, we've been working to improve on that now. I mean, it's certainly a big disparity that we do need to close the gap for. And so one of my other mentors, Dr. Joseph Evans, he and I are going to be working on improving our clinical workflow and making sure we are standardizing the assessment of sexual health in women up front, and as well as in follow up with patient reported outcomes and being a little bit more standardized about that.
I've also talked to our occupational therapy colleagues and physical therapy colleagues and our sexual health colleagues to open up those lines of communication and open up those referral pathways, so that hopefully we can be a little bit more knowledgeable and cognizant of the problem, and get women the help that they need. I think it's just helpful to have something tangible come out of research. Right? You don't want to just discover the problem and then let it be. Now it's kind of time to fix it.
Mary Clare Fischer:
Yeah. Yeah, I think that's amazing. That's so cool that you're really actively taking those results and putting them into some practice changes. What do you think would need to happen, in order to shift how research is conducted around sexual function for patients with cancer? You kind of mentioned a lot of patient care or clinical workflow changes. But I'm curious as to what you think about, how do we make sure that this is being studied more and in appropriate ways?
Dr. Jamie Takayesu:
That's a really good question. I think getting other young investigators excited and passionate about this is one thing. And just dissemination of information is always kind of the first step. I think I don't have a great answer in how to combat some of the bigger systemic issues surrounding biases regarding female sexuality. I think that's going to be decades worth of work, frankly.
But I do think that starting to talk about these problems a little bit more systematically and to try to bring these changes into clinic. And then to promote other researchers who are looking at female sexual health after radiation. And honestly, functional wellbeing and functional health after radiation, rather than just combating toxicity, but seeing how people's lives actually change after radiation. I think all of that type of work could really use a little bit more attention in our field.
Mary Clare Fischer:
What are the ways that you think that radiation oncology treatment needs to or could be able to shift, given your findings from this research?
Dr. Jamie Takayesu:
So I think aside from all of the physician assessment and other practitioner assessment, I do think there's quite a dearth of information regarding actual radiation treatments for gynecologic malignancy, specifically trying to again, preserve some of that functional anatomy and preserve [00:13:00] some of that sexual function. There are a couple of trials in the prostate space actually, that are looking at sexual preservation, and how can we modulate the radiation dose to decrease the dose to the structures that we think are related to erectile dysfunction after prostate radiation? So my dream would be to run a similar trial in the gynecologic space, trying to modulate radiation dose to structures that are important for female sexual function, and hopefully improves the outcomes for these women long term.
Mary Clare Fischer:
Anything else that you would like to add about this research?
Dr. Jamie Takayesu:
I think, again, this is something that I strongly believe every radiation oncologist knew intuitively, but just didn't quite have the data to point to, that this was a problem. And hopefully, this is an impetus for people to start asking women about their sexual health at the time of consult, at [00:14:00] follow ups. And hopefully just raise awareness that women do want to be asked about these things, and that they do need more care that we're not providing.
Speaker 1:
Thank you for listening, and tell us what you think of this podcast by rating and reviewing us. To stay up to date on what's happening in the cancer world, follow us on Twitter @UMRogelCancer. You can explore additional episodes at www.rogelcancercenter.org/podcasts. [00:14:30] Cancer Wise is part of the Michigan Medicine Podcast Network.

Listen to more Cancer Aware podcasts - a part of the Michigan Medicine Podcast Network.