A surgeon takes on educating the next generation
5:00 AM
Author |

Jeffrey Punch, M.D., a transplant surgeon at University of Michigan Health, has his week-long trips to Rwanda down to an efficient science.
He brings just one bag, a carry-on typically packed with a week's worth of underwear, socks and shirts, a jacket, three pairs of pants, a shaving kit and loupes.
The pants are worn twice each to save on packing space.
A mini pharmacy also collects frequent flier miles in case travel-related illness strikes.
It’s not a lot, but it’s enough, and it’s best to keep things simple for ease of repeating.
That’s how he approaches the kidney transplant program he’s helping to start there: Teach a few, use existing resources, help many.
The road to Rwanda starts in Ethiopia
Punch started his work in Africa through his church, doing mission trips to Kenya.
The trips were quick in-and-out visits that did not involve direct patient care.
Punch’s group provided local youth with basic medical education, such as CPR and sexual education, that was not typically covered in primary and secondary school curriculums.
“It was basically volunteer work, the kind of mission stuff that is not really sustainable, but was a lot of fun,” Punch said.
What was sustained was the connection to the country.
The people and the setting got him hooked on Africa.
Along came a Michigan trainee and chance to do something that didn’t just feel good but could do lasting good. It would also fit his skill set as a transplant surgeon.
Senait Fisseha, M.D, J.D., hailed from Ethiopia and obtained her medical and law degrees in the United States. She then trained as a resident in Obstetrics and Gynecology at University of Michigan Health and secured a grant from the Susan Thompson Buffett Foundation to address women’s health issues in her home country.
As Fisseha worked on programs within her own specialty, she learned the prime minister wanted to start a kidney transplant program to tackle a growing and expensive chronic kidney disease problem–a paradox of the expanded Ethiopian life expectancy.
Different and more chronic conditions can plague a population as it ages overall, and Ethiopia was no exception.
Conditions like kidney disease were competing with tropical diseases as drivers of morbidity and mortality and the government was sending people abroad for treatment and transplants at great expense.
Supplies weren’t enough.
The country needed trained specialists to manage the problem at home, and they needed to learn at home for the program to succeed.
“What they really need is to learn. We're recognizing that bigger hospitals that do more surgery have better outcomes in most cases,” Punch said.
“To meet the standard of a high-quality transplant program, you can't just bring it in and drop it into place. It must be developed in place.”
Fisseha tapped Punch through help from Tim Johnson, M.D., then the chair of the obstetrics and gynecology department at University of Michigan Health, who had also done extensive work in Africa with the goal of education and training of specialists in their home country, rather than the traditional model of showing up on mission trips, doing operations, and then leaving.
Punch and others partnered with St. Paul’s Hospital Millennium Medical College in Ethiopia’s capital city of Addis Ababa, making numerous trips starting in 2013 and training four surgeons.
The process taught Punch about navigating an unfamiliar bureaucracy, a different culture and different approaches to care.
A less direct culture demanded patience, and an investment in time.
The communication barriers were less linguistic than stylistic.
To meet the standard of a high-quality transplant program, you can't just bring it in and drop it into place. It must be developed in place.”Jeffrey Punch, M.D.
Where the Americans wouldn’t hesitate to get to the point or state that something wasn’t working well, the Ethiopians might hedge to avoid disappointing anyone.
Limited access to supplies made trust and respect for local practices paramount.
Case in point: When Punch learned they didn’t have oral narcotics for post-operative care, he didn’t think they could operate.
“They said, ‘Don't worry, it'll be fine, you'll see.’ I trusted them on that, and it was amazing to see how well people did without narcotic analgesia. This was at the time we were recognizing how bad the opioid epidemic was in this country,” Punch said.
This experience helped spur opioid-sparing policy work along in Michigan, according to Punch.
The Ethiopia program took six years to stand up and is now self-sustaining, though not immune from disruption: The COVID-19 pandemic and a civil war have both periodically paused the program.
Same need, different country
Fisseha’s work later took her to Rwanda, where the same problem existed for kidneys.
Having essentially finished his work in Ethiopia, Punch followed, this time partnering with more healthcare providers to stand up a program based at King Faisal Hospital in the capital city of Kigali.
He first touched down in Rwanda in 2022 and has been returning every six weeks since May 2023.
In addition to his carry-on, Punch usually travels with a nephrologist and a social worker. The nephrologist helps manage the physical condition. The social worker helps ensure conditions outside of the body are conducive to a successful transplant—for example, that potential organ recipients have adequate support at home and a clean, safe place to sleep and recover. The patients also need to be able to obtain and take their critical immunosuppression medications for the kidney to survive.
That part can be tricky to get right. Potential recipients, understandably eager for a new kidney, aren’t always up front about their home conditions, and the team needs to balance the risk with the reward.
“They'll claim to have a place to sleep, and it turns out they do, but the place they sleep is on a mattress with two other people. And then what if there's only a dirt floor? Is that okay? Can a transplant patient live there? We don't really know,” Punch said.
“It's never really been done before. We don't want to deprive someone of a transplant that could succeed, but we don’t want someone that's going to die of infection three months after the transplant.”
A special kind of cultural competency is needed in Rwanda. The brutal 1994 genocide that resulted in the death of nearly one million ethnic Tutsi and moderate Hutu left deep mental wounds for many Rwandans. The team is working with local psychiatrists to ensure recipients are mentally prepared for the procedure and recovery.
“The psychiatrists work on the mental health piece because it's an important component. People with these chronic diseases are frequently depressed,” Punch said.
“There's a huge amount of PTSD in Rwanda among the genocide survivors and we know that patients that have mental disorders don't do well with something like a kidney transplant.”
Punch learned from the Ethiopia experience to scale down the training; instead of training four surgeons as he did in Ethiopia, he planned to train two to stand the program up quicker.
As it turned out, one of the surgeons broke her ankle partway through training, so another was recruited to train. In the end, three people will be trained.
Michigan Medicine trainees are also learning.
Joy Obayemi, M.D., a general surgery resident, has family ties in Nigeria and has always wanted to tie Africa into her medical practice. As a medical student on the interview trail at University of Michigan Health, she shared her vision and a faculty member directed her to Punch.
What they really need is to learn. We're recognizing that bigger hospitals that do more surgery have better outcomes in most cases." Jeffrey Punch, M.D.
She remembers that he was humble and that he minimized his work, in contrast with her awed reaction. She ultimately matched at Michigan Medicine and kept tabs on Punch’s work in Africa.
“When I was a first year, I picked his brain about it. As a third year, I picked his brain about it more and said I would really love to be involved. I think at that point I just wore him down,” Obayemi said through a smile.
They traveled to Rwanda together in January of 2024.
Obayemi’s experience was mostly hands-off; she knew that parachuting in and jumping into cases would be an abuse of her privilege and could eat into valuable training time for local trainees.
She gained valuable exposure to an environment with a different set of resources and saw how it forces more intention. Limited access to suture material, for example, might change the operative approach to conserve the supply.
At the macro level, the trip exposed her in a very raw way to how systems work—training not seen in a typical rotation in most residency programs.
“We go from surgery, rotation, surgery, rotation and we don't really know how it all comes together. These opportunities force you to ask those questions and to try to understand how the system works in a totally new context, a new country, a new hospital, to see different patient work flows to see different styles of hospitals,” Obayemi said.
A different world
On a spring day in Ann Arbor, Emmanuel Muhawenimana, M.D., stood at the edge of an operating room as a kidney was laparoscopically removed from a donor.
Muhawenimana, a urologist based at the Kigali University Teaching Hospital, is one of the trainees associated with the Rwandan program and was on his first visit to Michigan Medicine to learn and observe.
He is one of 13 urologists serving all of Rwanda, a country of 13.8 million people.
“No Scrubs,” a song by the hip-hop trio TLC, played in the room.
Attending transplant surgeon Meredith Barrett, M.D. and transplant fellow Tiffany Zens, M.D., mobilized and removed the healthy kidney and carried it to a nearby table to prepare it for transplant.
The team packed the cleaned-up kidney on ice in a plastic container, which was then swaddled in multiple plastic bags, placed in a cooler and walked down the hallway to a nearby operating room. In the room was the prepped recipient, the surgical staff and a da Vinci robot.
Danielle Haakinson, M.D., kicked off her shoes and took a seat about five meters away from the patient at the robot.
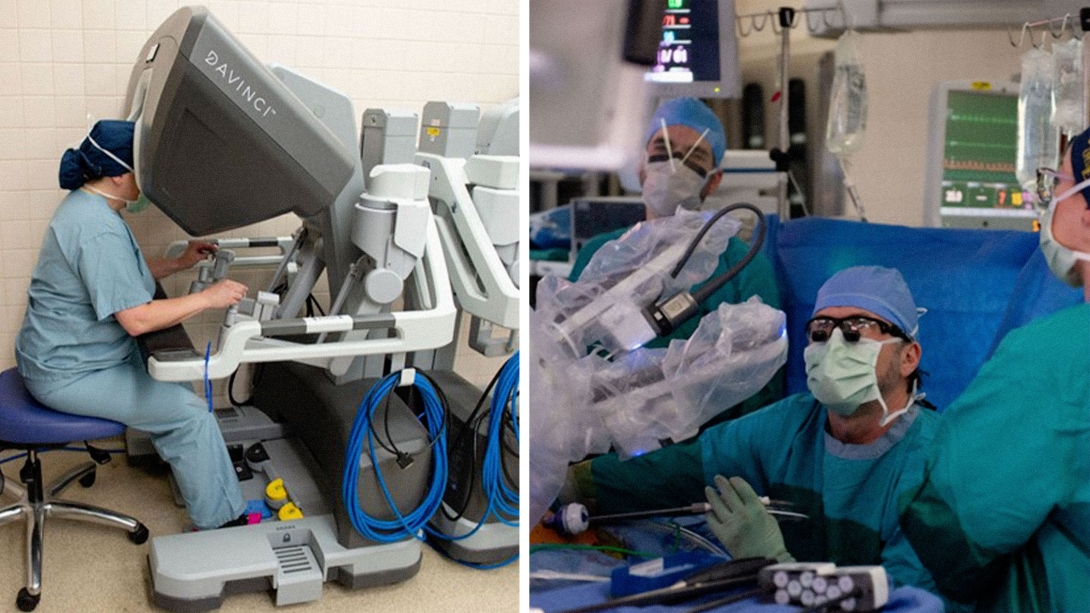
She looped her fingers into hand controls and operated it with small hand gestures and taps of her stocking feet.
Fellow transplant surgeon Chris Sonnenday, M.D., sat at the patient’s side to assist with placing the kidney via a larger incision and manually manipulating it as Haakinson connected structures.
He fed instruments, at Haakinson’s request, to the robot via ports inserted into the patient’s abdomen.
“Our most expensive equipment is the ice machine,” Muhawenimana quipped as the robot’s arms danced around the patient.
While his team won’t use the same tools, the principles were still the same, and shown in high-definition 3D: Expose structures, connect structures, make sure they function as hoped and close everything up.
Before long, the newly installed kidney spit a few drops of urine, a basic bodily function worth celebrating.
The hands doing the work at home would be flesh and bone.
There can be unintended consequences of training people on equipment they don’t have access to back home, according to Punch.
They may return frustrated because they can’t use their newfound skills or leave to practice in another country where such technical skills are in demand and there are resources to accommodate them.
The goal of the Rwandan program was to avoid contributing to brain-drain and focus on people, not platforms.
“You can do a lot of good with surprisingly minimal resources. In a place that lacks resources, even if there are a small number of people that can afford expensive things, it really doesn't have a big impact compared to serving the average man,” Punch said.
The impact so far on people in Rwanda has been profound.
As of May 1, 2024, the program had delivered 28 new kidneys to people who desperately needed them. In every case, a Rwandan surgeon did the transplant with Punch teaching them how.
At some point–Punch hopes by the end of 2025–the trainees will be able to fly on their own and Punch will lessen the frequency of his visits and eventually stop coming altogether.
He reflected on friends with different careers who have cool hobbies, like racing or restoring cars. Sometimes that seems enticing, but then he remembers the reward of coming home after giving four people new kidneys.
Of stepping out of the operating room and looking out over the impossibly green Rwandan mountainside, the home of so much pain and now so many miracles.
“Transplant’s so magical. Surgeons can often cure someone of cancer. But it's not like you take someone that's miserable, and make them feel well the next day. As weird as it sounds, patients that need an operation for a cancer often have a better quality of life than patients with kidney failure on dialysis. The effect of a living donor transplant can usually be felt by the patient immediately. They often feel dramatically better literally the next day, and the patients are extremely grateful.” Punch said.
And then there are the donors, who undergo surgery they don’t need to improve their own health.
They’re also grateful for the opportunity to help someone—usually a loved one.
“They are the true heroes. The trust the living donors show is remarkable and makes me feel good about the future for humanity,” Punch said.
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





