When cancer invades one breast, many women opt to remove both. Two new studies highlight the trend toward elective double mastectomy.
7:00 AM
Author |

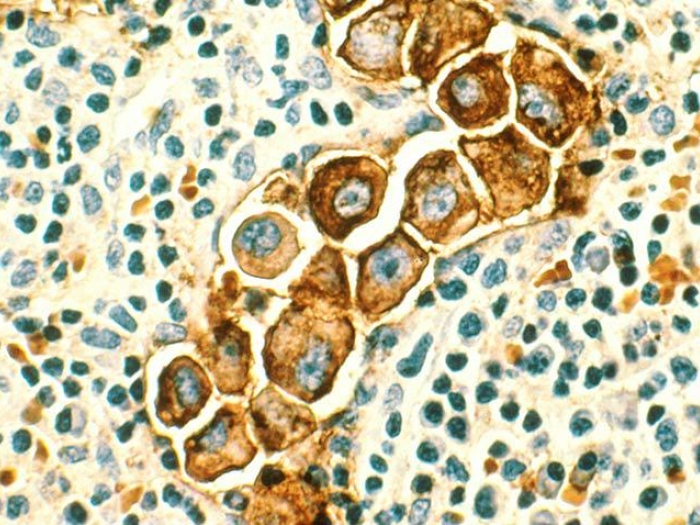
An increasing number of women diagnosed with cancer in one breast are choosing to have both breasts removed. The procedure, called contralateral prophylactic mastectomy, or CPM, has ignited a controversy within the medical community.
MORE FROM THE LAB: Subscribe to our weekly newsletter
On the one hand, doctors want to respect patients' treatment decisions and respond to those overwhelmed by worries of cancer returning. On the other, performing CPM on women at minimal risk of recurrence is considered by many to be overtreatment, driving more complications and greater costs to the health care system.
Adeyiza Momoh, M.D., and his colleagues recently published two papers seeking to understand patients' decisions and provide them with the right counsel. Momoh, a reconstructive surgeon in the University of Michigan Rogel Cancer Center's Breast Cancer Center, discusses what they found below.
What are the primary factors breast cancer patients consider when making treatment and reconstruction decisions?
Momoh: One thing every patient wants to know about is the risk of cancer returning. In women with cancer in one breast, the annual incidence of developing cancer in the other breast is less than 1 percent. Women at elevated risk are those with specific genetic risk factors, a family history or prior radiation to the chest wall. Although the statistics are reassuring, women must also grapple with the reality that their quality of life could be diminished if they are overly preoccupied or worried about cancer returning.
Another consideration is the risk of surgical complications. Generally speaking, the more significant the surgical procedure, the greater the risk, so removing and reconstructing two breasts is likely riskier than similar procedures for one. Other factors to weigh with surgery are body image and satisfaction related to breast appearance, symmetry and feel. It's far from an easy decision.
Since the chance of recurrence is so low, it seems like women would prefer the least risky and invasive option, correct?
Momoh: Surprisingly, at our academic medical center, even when presented with the rather encouraging news about recurrence, and even when educated about the risks associated with removing two breasts instead of one, many favor CPM.
The percentage of patients opting for CPM nationally has more than doubled in the last six years, from 4.2 percent to 11 percent. At the same time, the percentage choosing breast conserving procedures to treat early stage breast cancer has decreased.
Those electing CPM tended to base their decisions more on information from others, including survivors, rather than on their doctors' input.Adeyiza Momoh, M.D.
What does your new research reveal about CPM's surgical outcomes?
We recently published two studies exploring surgical outcomes, as well as how breast cancer patients make treatment decisions and how they felt about those decisions. The first study was performed through the Mastectomy Reconstruction Outcomes Consortium (MROC), a multicenter collaboration funded by the National Cancer Institute. It looked back at the experiences of 1,144 women from 11 hospitals in the United States and Canada between 2012 and 2014. All underwent either unilateral mastectomies (47 percent) or CPM (53 percent) with reconstruction. Some women had implant reconstructions and others used their own tissue for reconstruction.
SEE ALSO: Study Finds Double Mastectomy Tied to More Missed Work
As expected, more postoperative complications were observed after CPM and all forms of reconstruction.
Women who chose to have both breasts removed and have bilateral implant reconstructions experienced more preoperative anxiety than similar women who had one breast removed with subsequent implant reconstruction. After surgery, there was no difference in the anxiety levels of the women who had implant reconstructions, suggesting that, in the subset of women with implant reconstruction, those who chose CPM experienced a greater reduction in anxiety.
Women who chose CPM and implant reconstruction also had increased satisfaction with the results of their reconstruction when compared to women with unilateral mastectomy and implant reconstruction.
These differences in anxiety level and satisfaction were absent in groups of women (both CPM and unilateral mastectomy) who used their own tissue for reconstruction.
Explain the second study. What did it reveal about the decision-making process patients go through?
Momoh: To gain an appreciation for how women made decisions for CPM, we studied 30 patients treated here at U-M. While it was a smaller group, the breakdown was similar to the larger study — 43 percent chose unilateral mastectomy, 57 percent CPM.
Worry about recurrence was the No. 1 concern when women made decisions for CPM, even though patients acknowledged being informed about the actual risks. And, again, those expressing the most anxiety were those who chose CPM with many believing that they faced significant risks despite being told otherwise by their doctors.
While both groups were well informed, those electing CPM tended to base their decisions more on information from others, including survivors, rather than on their doctors' input. While their surgeons tended to recommended breast conserving surgery first and unilateral mastectomy second, nearly one-third of these patients admitted making up their minds before consulting with their physicians. Conversely, patients who chose unilateral mastectomy relied more on information and counsel from their physicians.
A desire for breast symmetry played a supporting role for patients choosing CPM. After surgery, women who chose CPM and reconstruction were more satisfied with their breasts than women with unilateral mastectomy and reconstruction.
However, it's important to note that overall, patients in both groups were pleased with their decisions and outcomes.
What do you want patients and physicians to learn from these studies?
Momoh: Even though CPM comes with higher complication rates and may not be an absolute medical necessity, this research shows that it may be the right choice for some patients, specifically for reasons of relief of worry.
With the existing complexity of information on breast cancer in general and this subject in particular, I hope that patients will rely more on physicians to help guide them through mastectomy and reconstruction decisions.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!