Urinary tract infections are a pain. A doctor explains how to banish them for good
5:00 AM
Author |

Listen to this episode on Health Lab's podcast page or wherever you follow your favorite podcast shows, like on Spotify and Apple Podcasts.
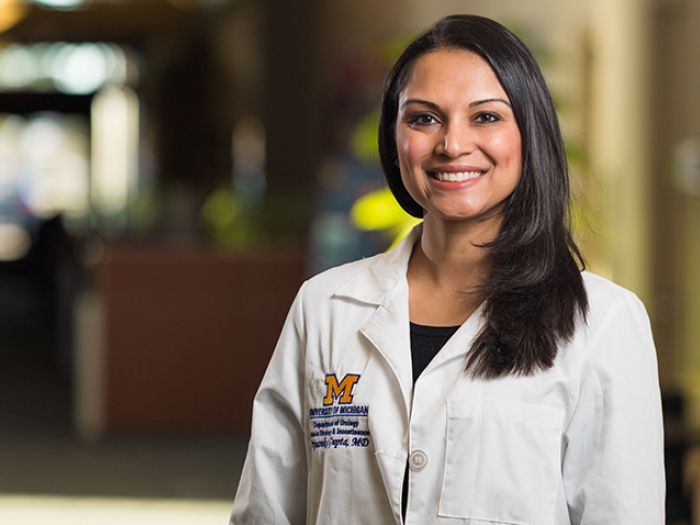
As a urogynecologist, Payton Schmidt, M.D., of University of Michigan Health Von Voigtlander Women’s Hospital, sees patients nearly every month for the same stubborn issue: a urinary tract infection.
A UTI occurs when bacteria grows somewhere along the urinary tract, whether it’s the bladder, urethra or kidneys.
About 40% of women experience one UTI in their lifetime. When it returns twice in six months, or three times in a year, it’s considered a recurrent UTI.
Recurrent UTIs are a common phenomenon, Schmidt says.
After a single UTI, 30–44% of women will have a recurrent UTI and 50% will have a third episode if they’ve had two UTIs in six months, she says, citing respected statistics from the journal Urogynecology.
Why are UTIs more common in women than men?
Women have shorter urethras than men do, so it’s easier for bacteria that’s hiding in the vaginal or rectal area to enter the bladder and multiply.
Menopausal women are more prone to UTIs, too.
The drop in estrogen causes changes in the pH of the vagina and in the urinary tract, which can allow UTI-causing bacteria to grow and trigger infections.
Symptoms of a UTI include:
- Burning while peeing
- Increased frequency to use the bathroom, often with little production
- Pain or pressure in the back, pelvis or lower abdomen
- Bloody urine
- Worsening urinary urgency or urinary incontinence
Why do UTIs reoccur?
Researchers continue to study the cause of recurrent UTIs and preliminary findings suggest several theories, Schmidt says.
In some cases, there’s a hereditary component to it.
When clusters of females in a family have repeated UTIs, it indicates there’s something different about their anatomy or immune system that causes them. It may be that their bacteria-fighting cells are weak at staving off UTIs, she says.
Or it may be both.
Women with pelvic floor disorders, incontinence, or even kidney stones, which may make it difficult to completely empty your bladder, tend to have recurrent infections.
The longer the urine stays, bacteria easily multiplies. This happens with men with enlarged prostates, too.
Another theory is that bacteria and host factors create environments where E. coli – the bacteria that causes most UTIs – creates a biofilm, which allows bacteria to persist in the bladder despite treatment with systemic antibiotics.
Other risks for a returning UTI include being sexually active, using a spermicide, having recent pelvic surgery or using a catheter to urinate.
Can poor hygiene cause a UTI?
While bacteria can grow anywhere, Schmidt stresses that wearing sanitary pads or incontinence pads too long isn’t the likely culprit of a UTI.
“There isn’t any convincing evidence that recurrent UTIs have anything to do with hygiene practices,” she said.
She won’t let patients think that either.
“I avoid letting patients get into that mindset because I don’t want them to think that this is something they did wrong.”
Nor does she dictate her patients only wear cotton underwear or loose-fitting styles for breathability – there’s no compelling evidence that suggests these are causes, she says.
How do you prevent recurring UTIs?
Hydration is key in keeping UTIs away. Schmidt recommends consuming 1.5 liters or more of water each day to flush bacteria out of the body as a prevention technique.
Schmidt also notes evidence around drinking cranberry juice or taking cranberry supplements as a prevention method.
“It’s more prevention than it is treatment for one,” Schmidt said.
Urinating before and after sex is recommended as well. Intercourse may move bacteria from the vagina into the urethra.
If menopausal, topical use of vaginal estrogen can reduce urinary tract infections by 50% or more. It’s often the first line of defense in older women, she says.
Wiping front to back, especially after a bowel movement, prevents rectal bacteria from entering the vagina and urethra as well.
D-mannose, an over-the-counter supplement marketed for urinary tract health, is another choice to prevent recurrent UTIs. D-mannose is naturally found in fruits and berries, including cranberries.
Research shows that it saturates E. coli structurers, blocking them from adhering to urinary tract cells, which cuts down on instances of bacteria multiplying.
Methenamine is another preventive medicine.
It reduces or changes the pH in the bladder to make it more of a hostile environment for UTI-causing bacteria to grow. It’s one that Schmidt uses on patients who want to avoid the use of antibiotics regularly for prevention.
How do you treat UTIs?
Once you get a urine culture test, a physician identifies the bacteria that’s causing the infection and prescribes an antibiotic that will best tackle it.
Often with recurrent UTIs, you can take a low-dose antibiotic for a minimum of six months and up to two years to stop them, which has about a 95% success rate, says Schmidt.
Another option is taking a prophylactic antibiotic after sex if intercourse is a trigger for your UTI.
With treatment, we can help women significantly reduce how often they are getting UTIs.” Payton Schmidt, M.D.
And for those in menopause, vaginal estrogen therapy may also help.
“With treatment, we can help women significantly reduce how often they are getting UTIs,” Schmidt said.
What’s new in UTI research?
New innovations in treatment for UTIs are underway, Schmidt excitedly points out.
One in particular? More researchers studying biofilms.
Biofilms are cells that anchor bacteria to the surface. This allows bacteria to be more resilient to antibiotics and is a cause of persistent infections. Biofilm research could lead to a better understanding of the biofilm disease process, which will hopefully lead to the development of new prevention and treatment options.
Multiple researchers are also investigating E. coli vaccinations.
One randomized controlled trial currently underway is by GlycoVaxyn, a Swiss company, that has developed a multivalent bioconjugate vaccine for the prevention of E. coli infections. The company is re currently enrolling patients with recurrent UTIs.
Additionally, investigation is underway on instillations of different antibiotics, such as gentamicin, being put directly into the bladder. If this method is effective in preventing UTIs, the tactic could help reduce systemic side effects of antibiotics and also reduce the risk of antibiotic resistance because of how it’s solely isolated to treat the bladder.
Opening up the conversation around UTIs
Surprisingly, for as common as they are, “recurrent UTIs are still not something that are talked about a lot,” Schmidt said.
Schmidt plans to change this by raising awareness as an expert in pelvic floor disorders and urinary incontinence, as well as in her role as a clinical assistant professor in obstetrics and gynecology at the University of Michigan Medical School.
“There are people whose lives are really impacted by their frequent urinary tract infections,” she said. “And I’m here to help patients and educate more people on the topic.”

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!