Diabetes care providers should account for impacts caused by financial insecurity, researchers suggest
10:30 AM
Author |

Actively managing diabetes is crucial to preventing long-term health complications, but rising costs are creating barriers to treatment.
Diabetes is currently the most expensive chronic disease in the nation, according to the Centers for Disease Control and Prevention. The total cost of diabetes in 2022 was over $400 billion, accounting for one of every four health care dollars spent in the U.S.
According to a Michigan Medicine study published in Diabetes Research and Clinical Practice, people with diabetes, particularly those with type 1 diabetes, endure substantial out-of-pocket expenses compared to people without diabetes.
Using a national health care insurance claims database, researchers matched subjects with similar demographics, ensuring comparable populations with type 1 diabetes, type 2 diabetes and without diabetes.
Investigators tracked total and out-of-pocket costs between 2009 and 2018, as well as the amounts going toward medications, diabetes-related supplies, visits to providers, hospitalizations and emergency department visits.
The team found that type 1 diabetes had the greatest total and out-of-pocket costs — $25,652 and $2,037, respectively — in 2018.
Type 2 diabetes followed closely in both total and out-of-pocket costs, but there was a significant decrease in those without diabetes, who paid an average of $14,220 in total and $1,122 in out-of-pocket expenses.
From 2009 to 2018, total costs increased for all three groups, but only those with type 1 diabetes experienced a growth in out-of-pocket expenses.
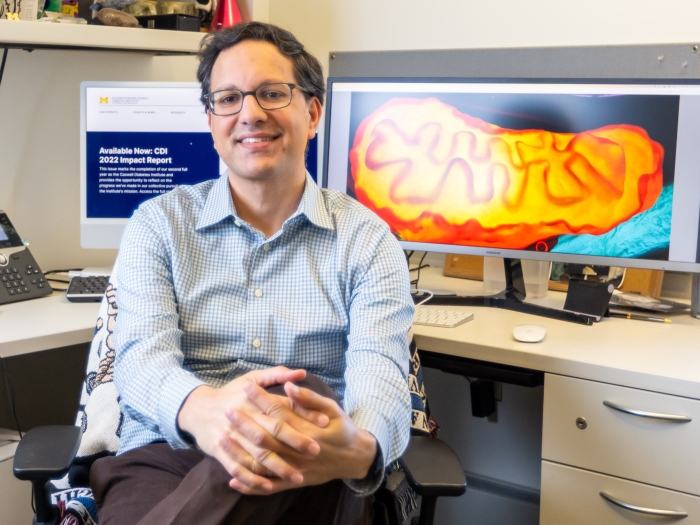
“If the trends we observed continue, people with type 1 diabetes will be facing increasingly unaffordable out-of-pocket costs,” said first author Evan Reynolds, Ph.D., lead statistician for the NeuroNetwork for Emerging Therapies at Michigan Medicine.
The rising price of medications is the main contributor to this trend, accounting for the largest portion of out-of-pocket costs, regardless of diabetes status.
Antihyperglycemic medications in particular, such as insulin, have steadily increased in price for both type 1 and type 2 diabetes.
“Studies show that the more a patient pays out-of-pocket, the less likely they are to stick with their medication long term, which poses a serious risk to their health,” Reynolds said.
In addition to expensive medications, people with type 1 diabetes are also facing an increase in the cost of diabetes management supplies, such as syringes, pumps and diabetic test strips.
“We worry about the inability of patients to afford any preventative health care services,” said senior author Brian Callaghan, M.D., a neurologist at University of Michigan Health and the Eva L. Feldman, MD, PhD, Professor of Neurology at U-M Medical School.
“Preventative measures for diabetes are not only effective for health but can save money in the long run.”
The out-of-pocket costs of these treatments can be crippling for patients, researchers say, leading to financial toxicity.
“Financial toxicity is when medical expenses begin to negatively affect all areas of a patient’s life, impacting both their physical and mental health,” Reynolds said.
“Diabetes care providers should be actively screening for the side effects of these costs, looking for signs of depression or anxiety.”
People living with type 1 diabetes are particularly at risk of financial toxicity. The first step to combating this? Curbing the costs of anti-hyperglycemic medications, Reynolds says.
“We need to enact policies that will either reduce or stabilize out-of-pocket costs and encourage people to properly treat their diabetes,” he said.
“With medications coming out on top in cost and utilization, lowering insulin prices is imperative right now.”
Additional authors: Kara Mizokami-Stout, Lynn Ang and Rodica Pop-Busui, Department of Internal Medicine, Division of Metabolism, Endocrinology, and Diabetes, University of Michigan. Nathaniel Putnam and Mousumi Banerjee, Department of Biostatistics, University of Michigan. Dana Albright and Joyce Lee, Department of Pediatrics, Division of Pediatric Endocrinology, University of Michigan.
Funding/disclosures: Dr. Lee is on the medical advisory board for GoodRx. Dr. Pop-Busui receives research support from Metronic, Novo Nordisk, and consults for Novo Nordisk, Regenacy, Roche, Procter &Gamble, Averitas and Nevro. Dr. Feldman consults for Biogen. Dr. Callaghan consults for DynaMed, receives research support from the American Academy of Neurology and performs medical legal consultations including consultations for the Vaccine Injury Compensation Program.
Citation: "“Cost and utilization of healthcare services for persons with diabetes,” National Library of Medicine: National Center for Biotechnology Information. DOI: 10.1016/j.diabres.2023.110983

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.