The discovery could lead to new treatments for metabolic diseases with fewer side effects
12:46 PM
Author |

Obesity is a complicated condition, caused by a combination of genetics, the food environment, behavior, and other factors.
For millennia, getting enough food to survive and thrive was difficult. For most people, it’s now as easy as opening a refrigerator.
A gene called SH2B1 has been shown to play an important role in regulating food intake.
SH2B1 mutations in people are associated with obesity, type 2 diabetes and metabolic dysfunction-associated steatotic liver disease, formerly known as non-alcoholic fatty liver disease.
“This gene controls feeding and energy expenditure. Obesity is caused by two opposing axes: If you eat too much, you gain fat. Spend too little energy and fat accumulates,” said Liangyou Rui, Ph.D., Department of Molecular & Integrative Physiology and the Elizabeth Weiser Caswell Diabetes Institute at the U-M Medical School.
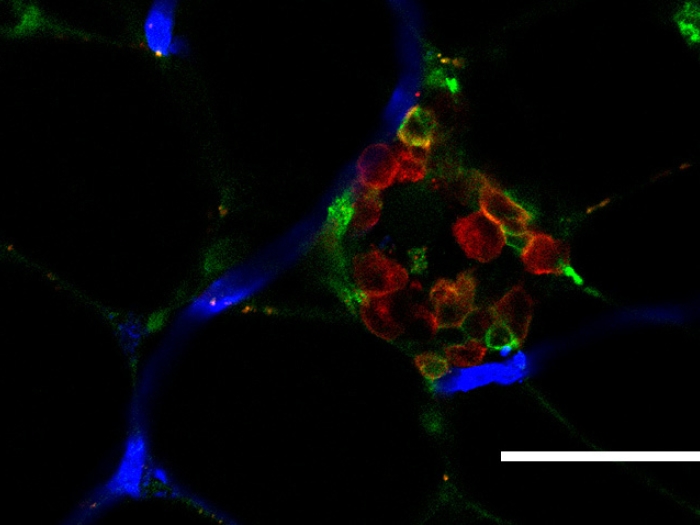
A study from Rui and team identifies where this gene is acting inside the brain, an area called the paraventricular hypothalamus, or PVH, which is involved in regulating blood pressure and fluid balance.
Additionally, the team discovered that neurons that express SH2B1 create a circuit, talking to neurons downstream in an area known as the dorsal raphe nucleus, located in the brainstem.
This area is implicated in energy balance and body weight maintenance and emotion motivated behavior.
Stimulating this circuit suppresses appetite in mice. Conversely, silencing the SH2B1 expressing neurons in the PVH leads to obesity.
The team also uncovered the molecular mechanism behind how SH2B1 helps maintain weight, in part by enhancing BDNF/TrkB signaling, which during development promotes brain growth and in a mature brain, maintains brain health. When this signaling goes awry, obesity and metabolic disease develop.
One theory, Rui notes, is that the inflammation associated with weight gain can negatively affect this pathway in an indirect way, weakening the signals to stop eating.
“We know that SH2B1 action is important, as it is highly conserved across species, from the fruit fly to humans,” said Rui.
“It functions as sort of a universal currency, not only enhancing cell signaling, but the hormones leptin and insulin, which help regulate appetite and metabolism.”
Furthermore, there have so far been no identified side effects to enhancing SH2B protein, unlike currently popular drugs, such as Ozempic or Mounjaro, that activate glp-1 receptors.
Said Rui, “If we can find a way to enhance SH2B activity, there is huge promise for treating obesity and its related diseases.”
Additional authors include Yuan Li, Min-Hyun Kim, Lin Jiang, Lorelei Baron, Latrice D. Faulkner, David P. Olson, Xingyu Li, Noam Gannot, Peng Li.
The Michigan Research Cores on this work include Metabolic, Physiological and Behavioral Phenotyping Core, Michigan Metabolomics and Obesity Center and the University of Michigan Center for Gastrointestinal Research
Paper cited: “SH2B1 Defends Against Energy Imbalance, Obesity, and Metabolic Disease via a Paraventricular Hypothalamus→Dorsal Raphe Nucleus Neurocircuit,” Advanced Science. DOI: 10.1002/advs.202400437
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!