A team of researchers use a unique ratio to uncover the causes of these mysterious conditions
12:02 PM
Author |

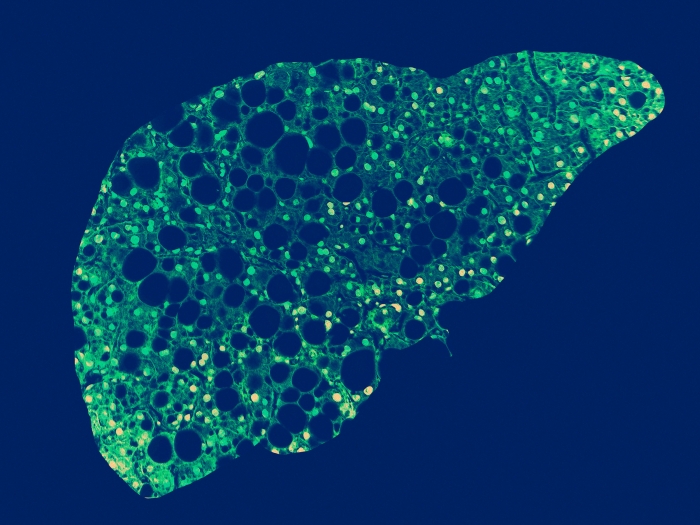
Insulin resistance has long been identified as the cause of diabetes, but many are unaware that it can also predispose some forms of cancer and other metabolic conditions, like obesity, dyslipidemia, hypertension, cardiovascular disease and metabolic dysfunction-associated steatotic liver disease, or MASLD.
However, due to a relatively poor understanding of its causes, there are currently very few treatments for insulin resistance.
Insulin resistance remains “hard to study” from a research perspective, said Elizabeth Speliotes, M.D., Ph.D., M.P.H., who serves as a gastroenterologist at Michigan Medicine and professor of internal medicine and computational medicine and bioinformatics at the University of Michigan Medical School. She is a member of the Elizabeth Weiser Caswell Diabetes Institute.
“Studying this condition requires cumbersome and oftentimes expensive gold standard measures,” she said. “The condition is genetically influenced, but only a limited number of genes affecting this trait have been identified at this point in time.”
Studying genetic components
This gap in understanding of the pathophysiology of this central cause of many metabolic diseases inspired Speliotes and a team of fellow researchers to further study its genetic components. Their findings were recently published in Nature Genetics.
“In our study, we used a more easily measured proxy of insulin resistance, the serum triglycerides to high-density lipoprotein cholesterol, or TG:HDL-C, ratio,” said Antonino Oliveri, first author of the study and an analyst in Speliotes’ laboratory.
“Serum triglycerides and high-density lipoprotein cholesterol can be conveniently quantified with a blood test. Essentially, this helped us carry out a much larger study of an insulin resistance marker, surpassing the scale of previous genetic studies of similar markers.”
The team’s study involved 402,398 Europeans from the U.K. Biobank, an extensive biomedical database and research resource containing de-identified genetic and health data and biological samples.
In addition, they identified over 350 loci, or points, within the human genome that are associated with the insulin resistance measure TG:HDL-C.
“Given the practicability of the trait we used, our work involved a marked increase in loci in comparison to previous studies of insulin resistance markers, becoming the largest study of an insulin resistance marker and the only study about this trait to date,” said Oliveri.
“Of the over 350 loci, 114 were also associated with the less powered serum insulin levels, HOMA-IR, which stands for Homeostatic Model Assessment for Insulin Resistance, or the Insulin Sensitivity Index, affirming specificity to insulin resistance.”
Insulin resistance
The team also found that associated genetic variants identified adipose tissue, as well as various physiological systems, that were affected by insulin resistance.
“Cardiovascular, liver, musculoskeletal and female urogenital systems were enriched for expression of genes implicated by the associated insulin resistance variants,” said Ryan Rebernick, who is an M.D. and Ph.D. candidate at U-M and co-first author of the study.
“The implicated genes also highlighted insulin signaling and growth, metabolism and abnormal lipid homeostasis pathways. Specific insulin signaling and growth-related genes, including EP300, CREBBP, SMAD1, SMAD3, ESR1 and IGF1R. Therefore, these hold the potential to serve as new targets for understanding the disease.”
Rebernick added that “another highlighted pathway was related to serine and threonine signaling. And a third network that was identified was related to adipose biology.”
“A decreased amount of white adipose tissue and altered functionality can cause lipodystrophy and promote insulin resistance,” he said.
The researchers later went on to identify five new subtypes of disease based on the effects of the genetic variants with related metabolic traits.
“These subtypes included brain processes, insulin and insulin growth, carbohydrate metabolism, adipogenesis and lipid homeostasis,” said Oliveri.
“We found that most, if not all, genomic variants that cause metabolic syndrome overlapped with the triglycerides to HDL-C ratio genomic variants. Metabolic syndrome, a condition that includes obesity, diabetes, and lipid and blood pressure defects can also lead to liver and cardiovascular diseases.”
New insights
Speliotes, senior author of the study, noted that the causes of metabolic syndrome are still unknown, but added the team’s findings suggest a very strong link between the high triglycerides to HDL-C ratio, insulin resistance and metabolic syndrome.
“Before this study, we had extremely limited insights into what causes insulin resistance, as well as metabolic syndrome,” said Speliotes.
“But now, through this work, we have a much more robust understanding of the pathophysiology of these diseases. Ultimately, this will allow us to better identify and treat the causes of these conditions with greater efficacy and fewer side effects to alter the course of these common metabolic diseases, which is very exciting.”
Additional authors: Annapurna Kuppa, Asmita Pant, Yanhua Chen, Xiaomeng Du, Kelly C. Cushing, Hannah N Bell, Chinmay Raut, Ponnandy Prabhu, Vincent L. Chen and Brian D. Halligan.
Paper cited: “Comprehensive genetic study of the insulin resistance marker TG:HDL-C in the UK Biobank,” Nature Genetics. DOI: 10.1038/s41588-023-01625-2.
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!