Heart failure patients get back to a longer, more fulfilling life, thanks to VAD technology
11:10 AM
Author |

Over the years, the evolution of ventricular assist devices has led to significant improvements that have allowed heart failure patients implanted with the device to live longer and with an improved quality of life. In fact, 70% of University of Michigan Health VAD patients are living at least five years with the latest VAD technology, and many are celebrating 10 or more years.
Ventricular assist devices were first approved in 2010 by the FDA as destination therapy for heart failure patients who were not considered candidates for heart transplant surgery.
A VAD acts as a pump to help the heart distribute blood throughout the body. For destination therapy patients, VADs are implanted permanently as long-term support, with the goal of extending and improving the patient’s life. A VAD is surgically attached to the heart and is connected to a driveline that exits the body near the abdomen. The driveline is then connected to a small computer that keeps the pump working.
“The newest VAD technology provides safe support and allows patients to return to an active, independent lifestyle,” said University of Michigan Health surgeon Francis Pagani, M.D., Ph.D.
Previously too large to fit in the chests of many patients, VADS are now available in sizes appropriate for most adults. And once recommended for those with advanced heart failure, VADs are now being used to treat patients with earlier stages of the disease.
The newest VAD technology provides safe support and allows patients to return to an active, independent lifestyle.”
Francis Pagani, M.D., Ph.D.
“VAD technology has evolved over time for the better,” said U-M Health VAD Program manager Sarah Comstock. “With the newest technology, we see fewer VAD-related complications, allowing patients to live longer and enjoy fulfilling lives. Many VAD patients are able to work, attend school, travel and spend more time with family and friends.”
The U-M Health VAD team is committed to using the latest technologies to care for nearly 200 current patients, says physician assistant Angela Rose, PA-C. “It’s wonderful to see patients who are so ill to be active once again and do the things they enjoy.”
Many U-M Health VAD patients are celebrating 10-plus years on a ventricular assist device. Several of them share their thoughts about life with a VAD.
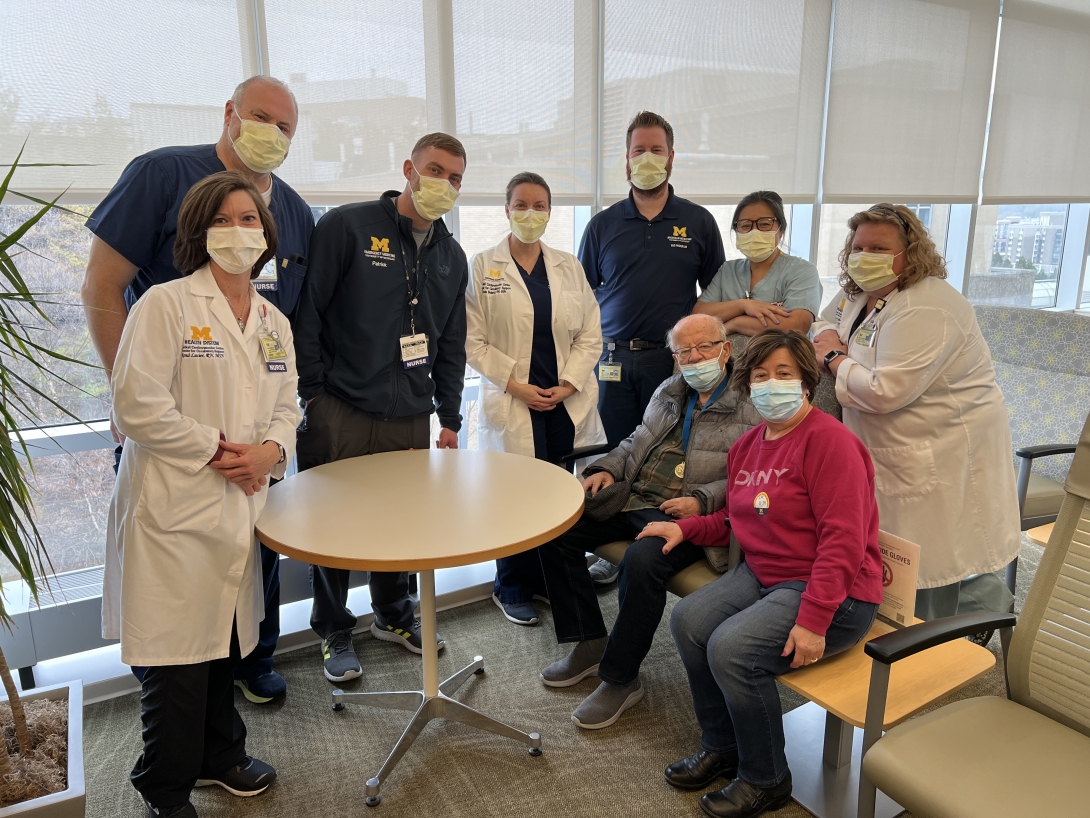
Dennis Foran, 82, of Clinton Township, MI, 12 years on a VAD
Pictured in main photo
“My VAD has done an amazing job keeping me alive. I’ve been able to lead a pretty normal life, despite a few other heath conditions not related to heart failure, and I can do pretty much anything. When I wake up in the morning I typically exercise for an hour. This and my VAD keep me going.”

“My VAD has given me extra time I didn’t think I would have to spend with family and friends. I’ve been here to see two grandchildren graduate high school and college, as well as the birth of my second grandson. I thank the wonderful U-M VAD team for giving me all the support through the years.”
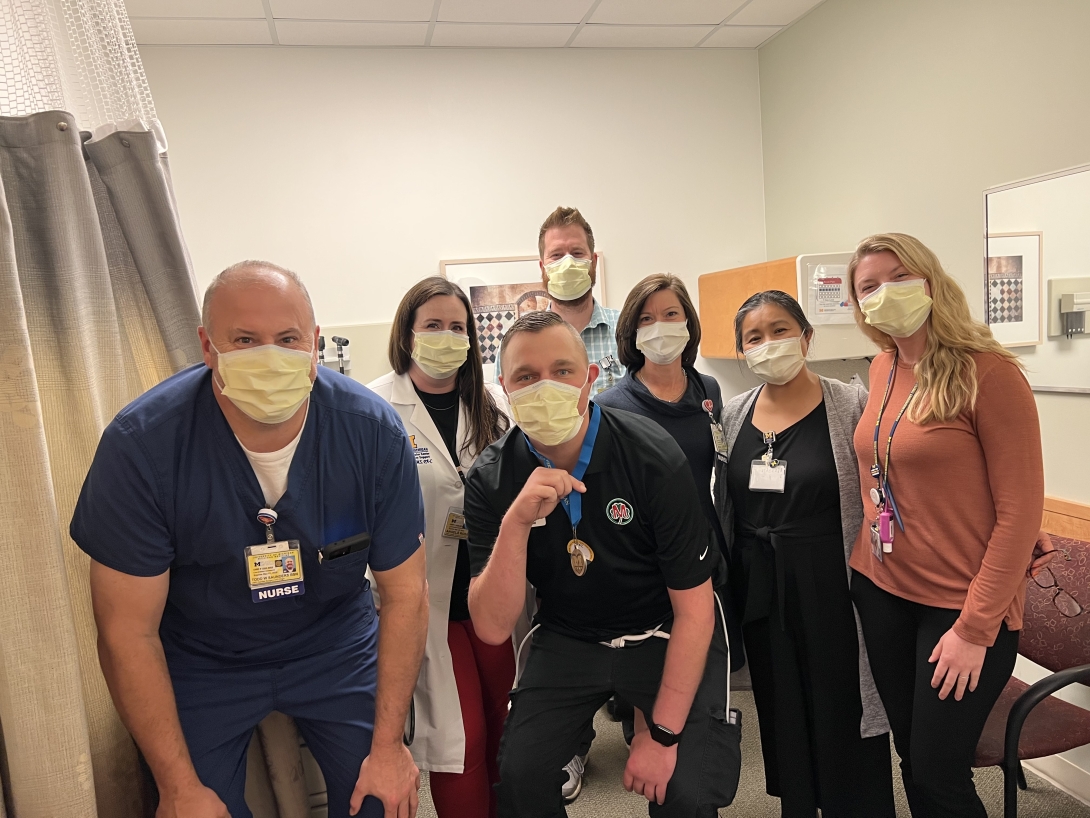
“I’ve been able to do things that wouldn’t be possible if it wasn’t for my VAD, like start a new career and coach my 14-year-old son, who was four when I first got my VAD. It took some time to get comfortable with the idea of a VAD, but I know mine is a good life to have. I’m now engaged and feel pretty blessed. Your life is not over if you have heart failure. You can do so much with a VAD.”
“I’m doing okay on a VAD and am living a pretty normal life. Dr. Pagani told me I was the only VAD patient who had traveled overseas with the device when I went to Greece in 2017 to visit my sister. He introduced me to a doctor there in case I needed help with my VAD. I don’t travel much now, but I try to stay active and walk every day. I thank God my doctors were able to keep me here.”

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





