Test looks at 18 genes, and was specifically developed to pick out cancers that need immediate treatment over the slow growing type, helping men avoid unnecessary biopsies
12:45 PM
Author |

Researchers at the University of Michigan Health Rogel Cancer Center have developed a new urine-based test that addresses a major problem in prostate cancer: how to separate the slow growing form of the disease unlikely to cause harm from more aggressive cancer that needs immediate treatment.
The test, called MyProstateScore2.0, or MPS2, looks at 18 different genes linked to high-grade prostate cancer. In multiple tests using urine and tissue samples from men with prostate cancer, it successfully identified cancers classified as Gleason 3+4=7 or Grade Group 2 (GG2), or higher. These cancers are more likely to grow and spread compared to Gleason 6 or Grade Group 1 prostate cancers, which are unlikely to spread or cause other impact. More than one-third of prostate cancer diagnoses are this low grade form. Gleason and Grade Group are both used to classify how aggressive prostate cancer is.
Results are published in JAMA Oncology.
“Our standard test is lacking in terms of its ability to clearly pick out those who have significant cancer. Twenty years ago, we were looking for any kind of cancer. Now we realize that slow growing cancer doesn’t need to be treated. All of a sudden, the game changed. We went from having to find any cancer to finding only significant cancer,” said co-senior study author John T. Wei, M.D., David A. Bloom Professor of Urology at Michigan Medicine.
PSA linchpin
Prostate specific antigen, or PSA, remains the linchpin of prostate cancer detection. MPS2 improves upon a urine-based test developed by the same U-M team nearly a decade ago, following a landmark discovery of two genes that fuse to cause prostate cancer. The original MPS test, which is used today, looked at PSA, the gene fusion TMPRSS2::ERG, and another marker called PCA3.
“There was still an unmet need with the MyProstateScore test and other commercial tests currently available. They were detecting prostate cancer, but in general they were not doing as good a job in detecting high grade or clinically significant prostate cancer. The impetus for this new test is to address this unmet need,” said co-senior author Arul M. Chinnaiyan, M.D., Ph.D., director of the Michigan Center for Translational Pathology. Chinnaiyan’s lab discovered the T2::ERG gene fusion and developed the initial MPS test.
To make MyProstateScore even stronger at identifying high grade cancers, researchers used RNA sequencing of more than 58,000 genes and narrowed it to 54 candidates uniquely overexpressed specifically in higher grade cancers. They tested the biomarkers against urine samples collected and stored at U-M through another major study, the National Cancer Institute’s Early Detection Research Network. This included about 700 patients from 2008-2020 who came for a prostate biopsy due to an elevated PSA level.
Narrowing the markers
This first step narrowed the field to 18 markers that consistently correlated with higher grade disease. The test still includes the original MPS markers, plus 16 additional biomarkers to complement them.
From there, the team reached out to the larger Early Detection Research Network (EDRN), a consortium of more than 30 labs across the country that are similarly collecting samples. This ensured a diverse, national sampling. Knowing no specific details about the samples, the U-M team performed MPS2 testing on more than 800 urine samples and sent results back to collaborators at the NCI-EDRN. The NCI-EDRN team assessed MPS2 results against the patient records.
Twenty years ago, we were looking for any kind of cancer. Now we realize that slow-growing cancer doesn’t need to be treated. All of a sudden, the game changed. We went from having to find any cancer to finding only significant cancer."
--John T. Wei, M.D.
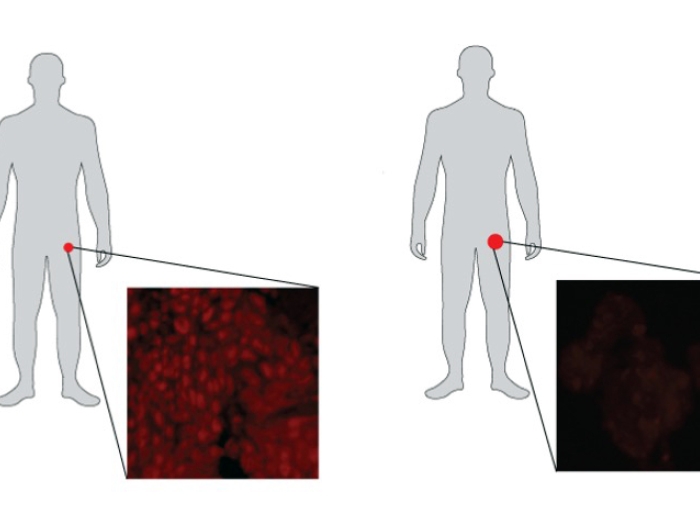
MPS2 was shown to be better at identifying GG2 or higher cancers. More importantly, it was nearly 100% correct at ruling out GG1 cancer.
“If you’re negative on this test, it’s almost certain that you don’t have aggressive prostate cancer,” said Chinnaiyan, the S. P. Hicks Endowed Professor of Pathology and professor of urology at Michigan Medicine.
Avoiding unnecessary biopsies
Moreover, MPS2 was more effective at helping patients avoid unnecessary biopsies. While 11% of unnecessary biopsies were avoided with PSA testing alone, MPS2 testing would avoid up to 41% of unnecessary biopsies.
“Four of 10 men who would have a negative biopsy will have a low risk MPS2 result and can confidently skip a biopsy. If a man has had a biopsy before, the test works even better,” Wei explained.
For example, a patient may get a prostate biopsy due to an elevated PSA, but no cancer is detected. The patient is followed over time and if his PSA inches up, he would typically need another biopsy.
“In those men who have had a biopsy before and are being considered for another biopsy, MPS2 will identify half of those whose repeat biopsy would be negative. Those are practical applications for patients out there. Nobody wants to say sign me up for another biopsy. We are always looking for alternatives and this is it,” Wei said.
MPS2 is currently available through LynxDx, which is University of Michigan spin-off company that has an exclusive license from the university to commercialize MPS2. Patients interested in learning more can call the Michigan Medicine Cancer AnswerLine at 800-865-1125.
Authors: The paper’s first authors are Jeffrey J. Tosoian, M.D., M.P.H., who is now at Vanderbilt University, and Yuping Zhang, Ph.D., and Lanbo Xiao, Ph.D., at U-M. Additional authors are Cassie Xie; Nathan L. Samora, M.D.; Yashar S. Niknafs, Ph.D.; Zoey Chopra; Javed Siddiqui; Heng Zheng, M.D.; Grace Herron; Neil Vaishampayan; Hunter S. Robinson, M.D.; Kumaran Arivoli; Bruce J. Trock, Ph.D.; Ashley E. Ross, M.D., Ph.D.; Todd M. Morgan, M.D.; Ganesh S. Palapattu, M.D.; Simpa S. Salami, M.D., M.P.H.; Lakshmi P. Kunju, M.D.; Scott A. Tomlins, M.D., Ph.D.; Lori J. Sokoll, Ph.D.; Daniel W. Chan, Ph.D.; Sudhir Srivastava, Ph.D.; Ziding Feng, Ph.D.; Martin G. Sanda, M.D.; Yingye Zheng, Ph.D.
Funding: From the Michigan-Vanderbilt Early Detection Research Network Biomarker Characterization Center and Data Management and Coordinating Center, which are through the National Cancer Institute grants U2C CA271854 and U24 CA086368. Additional funding is from NCI grants P50 CA186786, R35 CA231996, U24 CA115102, U01 CA113913; Prostate Cancer Foundation; Howard Hughes Medical Institute; and the American Cancer Society.
Disclosures: Chinnaiyan serves on the advisory boards of Tempus, LynxDx, Ascentage Pharmaceuticals, Medsyn therapeutics, Esanik and RAAPTA therapeutics. Tomlins is an equity holder and chief medical officer of Strata Oncology. LynxDx has obtained an exclusive license from the University of Michigan to commercialize MPS2 and the TMPRSS2-ERG gene fusion. Tosoian and Chinnaiyan are equity holders and scientific advisers to LynxDx. Siddiqui, Zhang, Xiao and Niknafs have served as scientific advisers to LynxDx.
Paper cited: “Development and Validation of an 18-Gene Urine Test for Clinically Significant Prostate Cancer,” JAMA Oncology. DOI: 10.1001/jamaoncol.2024.0455
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!