Multi-specialty team studying non-invasive method to measure underlying cervical tissue changes that precede birth
12:00 PM
Author |
During pregnancy, women often receive vaginal ultrasounds to measure the length of their cervix, helping predict their risk of delivering early – but this measurement is far from perfect.
Now, a team led by Michigan Medicine is using a novel technology to modify this routine prenatal test to collect more detailed information about the cervix to help precisely predict delivery time, and particularly, the risk of preterm labor.
A multi-specialty team of maternal fetal medicine experts and obstetric physicians, engineers and clinical research staff have developed a non-invasive imaging method showing underlying cervical tissue changes detectable in early pregnancy that precede preterm birth.
Specifically, the tool monitors cervical “ripening,” or stiffness and remodeling, the process by which the cervix shortens, softens, and dilates to allow passage of the fetus.
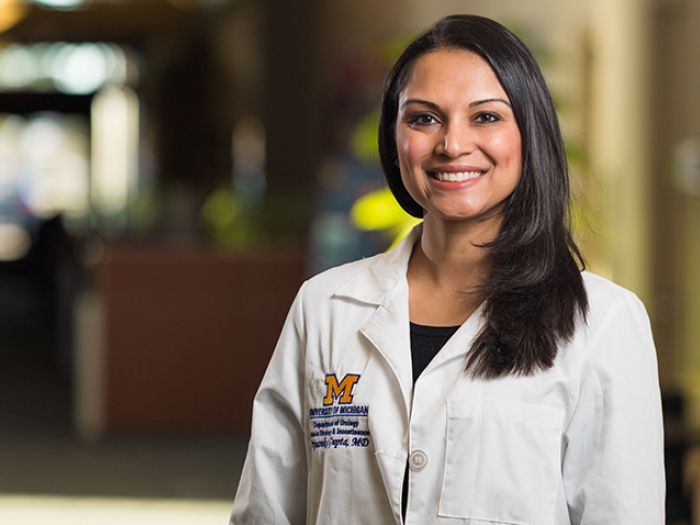
“Current methods to assess cervical stiffness have significant limitations affecting reliability,” says project lead Molly Stout, M.D., M.Sci., maternal fetal medicine director at University of Michigan Health Von Voigtlander Women's Hospital.
“Now we have a device that could be used to improve the prediction of preterm birth, allowing clinicians to better target interventions to people at risk.”
Stout and her team are presenting project milestones related to full-term birth at the 2024 Society of Maternal Fetal Medicine Pregnancy Meeting in Maryland.
She explains more about the team’s work:
Why do we need better ways to predict preterm birth?
Stout: Preterm, or premature birth, is when a baby is born too early, before the 37th week of pregnancy. This condition affects one in 10 births in the U.S and is a major contributor to neonatal death and lifelong adverse health outcomes. It’s also associated with billions of dollars in medical costs.
There’s a critical need to improve methods to correctly identify patients at risk for preterm birth to move both the clinical and scientific preterm birth field forward.
Currently, our inability to reliably predict when labor will occur is a significant barrier to solving this problem on a broad level.
Can you describe the device your team developed?
Stout: Our team invented a novel imaging tool we call a fully quantitative cervical elastography system (Q-CES), which modifies the standard transvaginal ultrasound probe to quantify both pressure and tissue deformation in the cervix.
This provides a system to fully measure cervical tissue stiffness that can be compared across patients for the first time, numerically describing this physiology just like we quantify and measure other things to define normal and abnormal states in modern medicine.
What are your newest findings related to full-term birth?
Stout: Although preterm birth is a major medical problem and has been the focus of our work to-date, we are also unable to predict the timing of birth as the due date approaches.
Our findings in late pregnancy suggest some promise at identifying cervical changes that may differ in patients with vaginal birth compared to those who ultimately require cesarean birth. We enrolled over 100 patients at 37 weeks or beyond and measured their cervical ripening weekly until delivery occurred.
We found that people with vaginal births demonstrated a 14% softening rate per week leading up to delivery whereas those with cesarean births do not soften. These are early findings, but we hope these measurements will open the door to identify opportunities to maximize the chance for vaginal birth in more people.
Overall, fully quantifying what is happening in the cervix, both at preterm gestational ages as well as at full-term will open new avenues for scientific advancement and clinical care in pregnancy.
This project received Frankel Innovation Initiative funding and an award from the Women’s Health Innovation Fund.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.