Research has many implications for patient management, inspired scientific statement from the American Heart Association
2:15 PM
Author |
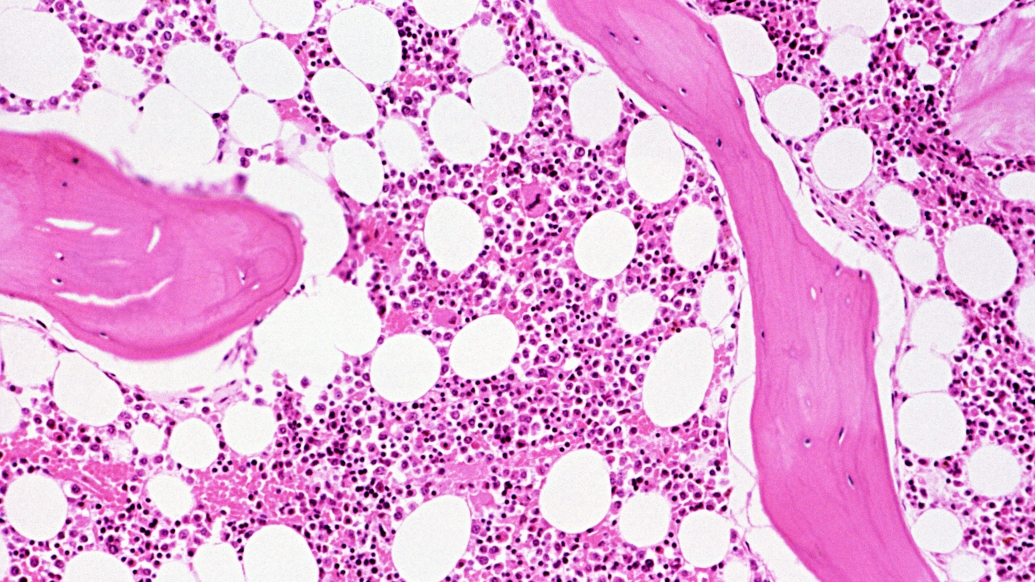
For thousands of Americans each year, a bone marrow transplant has the potential to cure diseases such as leukemias, lymphomas and immune deficiency disorders. While lifesaving, bone marrow transplants are taxing procedures that can affect various organs, including the cardiovascular system.
With advances in medical science and improvement in protocols, more bone marrow transplants, also known as hematopoietic stem cell transplantation, are being offered to older patients, a population at greater risk of cardiovascular disease.
Researchers led by Michigan Medicine have not only determined the contemporary prevalence of cardiovascular complications after bone marrow transplant — they developed a novel tool to predict a person’s risk for such problems following the procedure and help guide the pre-transplant process.
“In the early era of bone marrow transplant, patients with heart disease were often excluded due to the cardiotoxicity of the conditioning regimens used at the time,” said Salim Hayek, M.D., adjunct professor of internal medicine-cardiology at U-M Medical School who specializes in cardio-oncology.
“Understanding the cardiovascular risks of modern bone marrow transplantation is crucial for selecting the right patients and to ensure that none are excluded unnecessarily. This is the first contemporary evidence that shows the risks associated with bone marrow transplant and how to assess a patient’s risk for cardiovascular complications— which, taken together, can guide clinicians to ensure better outcomes for this procedure.”
Cardiovascular risks after transplant
Hayek and his team built the Cardiovascular Registry in Bone Marrow Transplantation, known as CARE-BMT, which compiles data of patients who underwent transplant from both University of Michigan Health and Rush University.
In a study of over 3,300 people who had a bone marrow transplant between 2008 and 2019, 4.1% of patients experienced cardiovascular events within 100 days after the procedure, and 13.9% did so after 5 years.
The results are published in JACC Cardio-Oncology.
SEE ALSO: How a healthy gut could lead to better bone marrow transplants
Rare complications
Overall, cardiovascular complications during the hospitalization for bone marrow transplant were rare. The most common short and long term condition was atrial fibrillation, with 6.8% of patients diagnosed at the five-year mark, followed by 5.4% of patients experiencing heart failure. Severe cardiovascular complications, such as heart attack and stroke, were uncommon.
Investigators also found that 16.4% of allogenic transplant recipients, those who received bone marrow from another donor, developed long term cardiovascular events after five years, compared to 12.1% of autologous recipients who had damaged bone marrow replaced with their own healthy blood stem cells.
“The landscape of bone marrow transplant has rapidly evolved over the last 20 years, with many improvements in the way patients are selected for and treated during bone marrow transplantation,” Hayek said.
“Our cohort allowed us to re-evaluate the incidence of cardiovascular complications in patients who received more modern treatment.”
Patients with preexisting cardiovascular conditions, such as diabetes and coronary artery disease, were more likely to have complications in the long term but not during the transplant process.
“Determining who is at high and low risk of cardiovascular outcomes is crucial to help guide both the pre-transplant evaluation as well as the post-transplant management — which is why we invested so much in creating a simple risk score that health care providers can use to identify these patients,” said first author Alexi Vasbinder, Ph.D., R.N., a post-doctoral fellow at the U-M Frankel Cardiovascular Center at the time the research was conducted.
Pre-bone marrow transplant risk cardiovascular score
To develop such a tool, researchers used data from the CARE-BMT cohort. They created a simple points based risk score using clinical information that is easily accessible, including age and race, history of coronary artery disease or heart failure, and prior doses of cardiotoxic chemotherapy medications.
In an analysis of just over 2,400 adult patients, the final risk model, now known as the CARE-BMT risk score, identified a high risk group that accounted for over 30% of the patients. The five year cardiovascular complication rate was 31.9%; that rose to 55% at 10 years.
The score performed equally well in allogeneic and autologous bone marrow transplant recipients, as well as in a separate cohort of over 900 patients from Rush University.
Results are published in the Journal of the American Heart Association.
“It’s a very simple score that can be easily calculated and implemented in any health care record,” Hayek said.
“This will be easy to replicate and use during evaluations before bone marrow transplant to guide referrals of high risk patients to cardiovascular specialists who can then optimize medical and lifestyle management of their conditions.”
AHA scientific statement
The two reports formed the basis of a scientific statement published by the American Health Association geared towards the cardiovascular management of patients undergoing bone marrow transplant.
The statement covers considerations during the four steps of hematopoietic stem cell transplantation : evaluation before transplant, conditioning therapy and transplant, immediate post-transplant period and long term survivorship.
“This innovative cardiac risk assessment tool significantly improves our ability to provide a safer path throughout treatment to our cell therapy recipients possessing cardiovascular comorbidities, which in turn will have a positive effect on long term recovery and quality of life,” said co-author John Maciejewski, M.D., Ph.D., bone marrow transplant physician at U-M Health and clinical assistant professor of internal medicine at U-M Medical School.
Additional authors: See links below.
Citations: “Cardiovascular Events After Hematopoietic Stem Cell Transplant: Incidence and Risk Factors,” JACC: CardioOncology. DOI: 10.1016/j.jaccao.2023.07.007
“Cardiovascular Risk Stratification of Patients Undergoing Hematopoietic Stem Cell Transplantation: The CARE‐BMT Risk Score,” Journal of the American Heart Association. DOI: 10.1161/JAHA.123.033599
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine

Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





