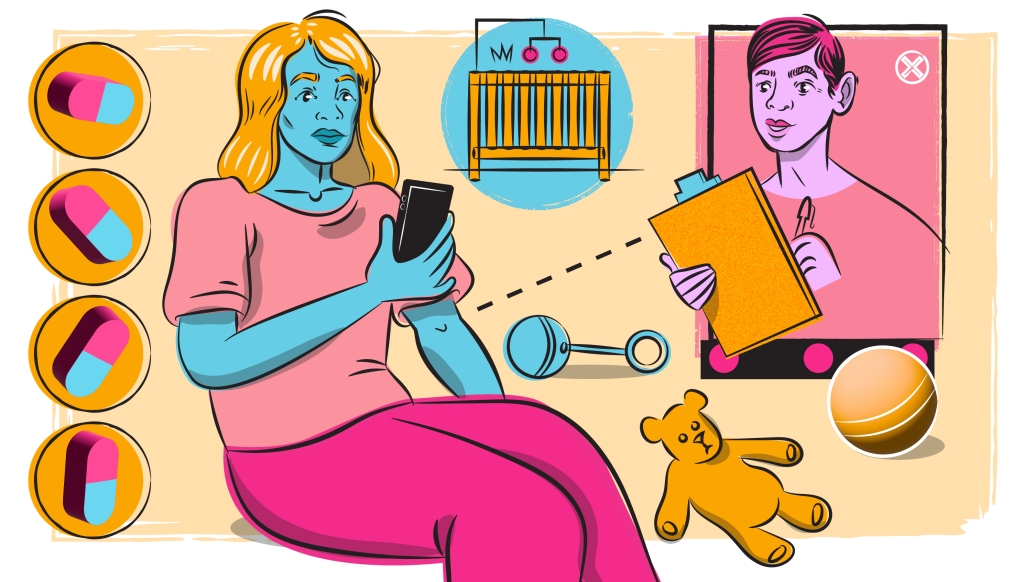
The fast-acting pill, paired with psychosocial treatment, offers a comprehensive treatment plan, but price concerns remain
5:00 AM
Author |
Listen to this article on Health Lab's podcast.
The first oral medication to treat postpartum depression, zuranolone (branded Zurzuvae), received approval from the Food and Drug Administration in August 2023.
Taken orally once a day for 14 days, the pill starts relieving depressive symptoms after about three days and the effects last up to 45 days.
Zuranolone supplies a mimic of allopregnanolone – a neurohormone that decreases rapidly after pregnancy – that acts on receptors to reverse the withdrawal effects that impact mood.
This mechanism differs from most anti-depressants, which target neurotransmitters and take up to six to eight weeks to take effect.
The fast-acting pill offers more convenience than the postpartum depression infusion treatment, brexanolone (branded Zulresso), which has been available since 2019, but cost concerns remain.
As with all mental health medications, zuranolone should be paired with psychosocial treatment to treat all factors contributing to the disease.
SEE ALSO: A $34,000 Drug for Postpartum Depression Brings Praise, Price Concerns
“We get excited about new medicines – which are wonderful – but we put a lot of resources towards developing medicines when known psychosocial risks need our attention as well. These risks often get forgotten and stay unaddressed,” said Maria Muzik, M.D., M.Sc., a professor in the Michigan Medicine departments of psychiatry and obstetrics and gynecology.
A ‘multifactorial origin’
Like during depressive periods at any other time in life, postpartum depression is characterized by symptoms such as low energy, sad or irritable mood, sleeping/eating too much or too little, or not feeling joy in expected activities, including caring for the baby. In severe cases, postpartum depression can be life-threatening as mothers may experience thoughts of harming themselves or their child.
SEE ALSO: Insomnia and Postpartum Depression: When a New Mom’s Sleep Loss Turns Perilous
Both biological factors, like the shift in the hormonal landscape after birth, and psychosocial factors contribute to the development of postpartum depression, says Muzik.
“Because postpartum depression has a multifactorial origin, we also need multilevel treatments. In clinical practice, we first address psychosocial factors with a wide range of evidence-based psychotherapies and support and then address biological factors with medications,” said Muzik.
Treating postpartum depression
Psychoeducation should come first, says Muzik. Women often don’t realize they are depressed or downplay their symptoms.
“Many women feel guilty for their depressive symptoms, and we must educate them that their symptoms are part of a treatable illness. They are not weak.”
SEE ALSO: A Third of New Moms Had Postpartum Depression During Early Covid
Peer-to-peer support groups, where moms support other moms, are enormously helpful. Psychotherapy, like cognitive behavioral therapy, interpersonal therapy, or parent-infant psychotherapy can help women work through their anxious or depressive feelings and support their parenting confidence while also developing strategies to avert future flare ups.
Until now, the mainstay of biological treatment for postpartum depression were anti-depressants or anti-anxiety medications that increased serotonin levels in the brain called selective serotonin reuptake inhibitors or SSRIs.
The newly approved zuranalone will offer another, mechanistically totally different, option for treating the biological underpinnings of postpartum depression.
“Postpartum depression co-occurs with anxiety even more so than major depressive disorder,” said Muzik.
“Zuranolone works on allopregnanolone receptors to decrease anxiety, insomnia, and depression associated with postpartum depression.”
Side effects of the medication include dizziness and sedation which prohibits patients from driving or operating machinery while taking the medication.
Patients cannot take the medication while pregnant and cannot breastfeed while taking the medication and for a week afterwards.
Importantly, zuranolone has an addictive potential and should be avoided in individuals with a history of addiction.
Cost concerns
It is not yet clear whether zuranolone will remain as costly as its intravenous predecessor, brexanalone.
Currently, zuranolone is FDA approved only for the treatment of postpartum depression and not for major depressive disorder.
Sage Therapeutics, the drug manufacturer, originally projected the price for zuranolone to stay under $10,000 if it was also approved for major depressive disorder. Now that the market is smaller, the price will likely increase.
If it’s not fully subsidized by Medicare or insurance companies, this medication will heighten health care inequities, says Muzik.
Those who can afford the medication or have insurance that covers it will have access and those who do not will not have access.
“I am very excited, but I also wonder what the ramifications are,” continued Muzik.
“My biggest concern is how will those who have the greatest risk and need get access to the medication?"
Resources
If you or someone you’re with is having a life-threatening psychiatric emergency, please call 911.
For mental health crises and urgent concerns, dial 988 for the National Suicide and Crisis Lifeline.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





