A cell therapy clinician talks about the treatment and its promising future to treat other diseases, too
5:00 AM
Author |
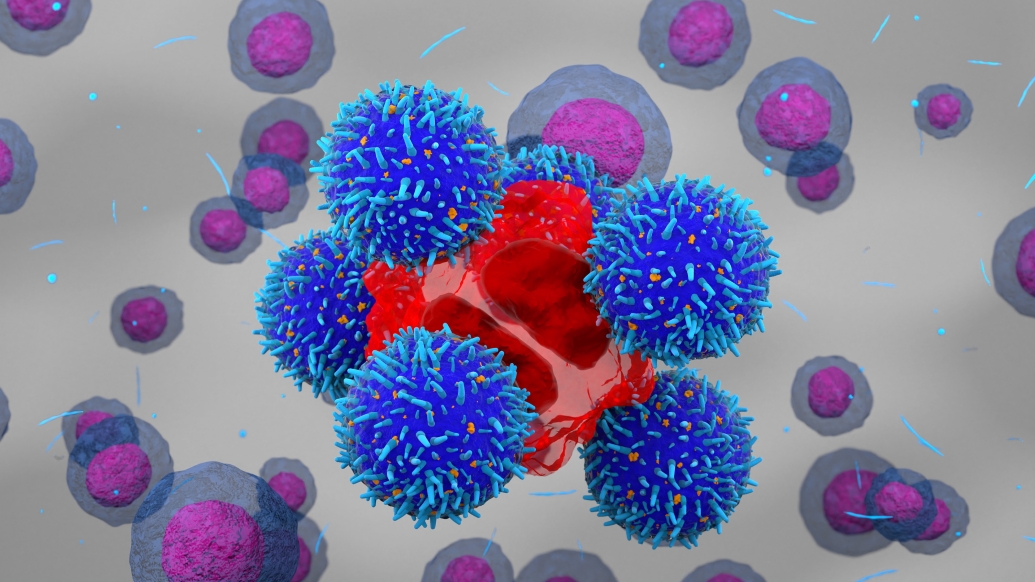
Advancements in using a person’s own cells to treat disease have been growing for years. These include developments such as precision medicine, immunotherapy and cellular therapy for blood cancers.
Most standard of care for treating blood cancers consists of using heavy doses of chemotherapy, which can cause a lot of side effects and not be as targeted.
But when using cellular therapy as a treatment, it doesn’t rely on chemotherapy to work.
Like chimeric antigen receptor therapy, your own body and immune system are used to target the cancer instead.
Here, Monalisa Ghosh, M.D., a hematologist-oncologist at the University of Michigan Health Rogel Cancer Center, discusses cellular therapy in regards to what it is, how it's unfolding and what exciting things are to come.
There have been many advances in treating blood cancer over the past few years. What are some novel treatments now in use?
Ghosh: Novel treatments for blood cancers including CAR T-cell therapy, small molecule inhibitors, checkpoint inhibitors, and bi-specific T-cell engagers, or BiTEs.
Most of these therapies use the patient’s own immune system to better target and treat the cancer.
How has CAR T-cell therapy informed future use for additional cancer types?
Ghosh: CAR T-cell therapy was first approved for acute lymphoblastic leukemia and non-Hodgkin’s B-cell lymphomas.
Due to its success in these blood cancers, the application of CAR T-cell therapies is broadening not only to other blood cancer types but also to solid cancers such as sarcomas, lung cancer, breast cancer, to name a few.
We have more knowledge of how to better manage the toxicities and adverse reactions associated with CAR T-cell therapy and are actively researching ways to improve CAR T-cell therapy function, safety and efficacy.
Other than CAR T-cell, what other cellular therapies are there? And are they only for cancer patients?
Ghosh: Most cellular therapies, such as CAR T-cell, are currently only available to cancer patients.
There are also FDA approved T-cell therapies for sarcomas as well as for melanoma.
Tumor infiltrating lymphocytes are a type of T-cell therapy that is FDA approved for melanoma.
Cellular therapy is now being used in the clinical trial setting for a variety of autoimmune diseases, though.
Recent data from Germany showed promising results using CAR T-cell therapy in patients with systemic lupus erythematosus, inflammatory myositis and systemic sclerosis.
Many autoimmune diseases are driven by the productions of autoantibodies by B-cells.
CAR T-cell therapy targeting B-cells can kill these autoreactive B-cells and improve symptoms of these diseases.
We don’t yet know if these diseases can be cured, but long drug-free remissions have been seen in some patients.
How has Michigan Medicine approached the use of cellular therapy?
Ghosh: Michigan Medicine has been at the forefront of the cellular therapy technology for over a decade.
We were a lead recruiting site in several of the initial clinical trials that led to FDA approval of CAR T-cell therapy in acute lymphoblastic leukemia and non-Hodgkin’s B-cell lymphoma.
Since cellular therapy is an extension of and was developed from the field of bone marrow/stem cell transplant, the oversight of cellular therapy at Michigan Medicine is maintained by the Bone Marrow Transplant Program.
We are also currently involved in multiple cellular therapy trials outside of cancer including in multiple sclerosis, systemic sclerosis and inflammatory myositis.
There are also upcoming trials in inflammatory bowel disease.
We have multiple CAR T-cell therapy and other cellular therapy trials in hematology/oncology.
What does the future hold for cellular therapy?
Ghosh: Cellular therapy will continue to have a broader application than we initially anticipated when this therapy was first developed.
With the emergence of cell therapy in autoimmune diseases, we will see a dramatic increase in the use of this technology, whether the cells are sourced from the patient or from a third-party donor.
We will continue to see improvements in cell therapy structure and functions, safety and efficacy, and manufacturing.
There have been rapid developments in shortening manufacturing time and in the use of third-party healthy donor “off the shelf” products.
In addition, gene editing technology has allowed for the development of novel cell therapy products to treat diseases such as sickle cell anemia.
The field is growing rapidly, and it's an exciting time to be a cell therapy physician.
Find out more about cellular therapy or call the Cancer AnswerLine at 800-865-1125.
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week.
Sign up for the Health Lab Podcast. Add us wherever you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine

Clinical Associate Professor
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!




